Best Exercises for Vestibular Rehabilitation: A Guide to Reducing Dizziness and Improving Balance
Dizziness, imbalance, and vertigo can significantly impact daily life for those with a vestibular disorder. Whether you’ve recently been diagnosed or are simply exploring potential causes for your symptoms, vestibular rehabilitation therapy (VRT) offers a path toward improvement. VRT consists of targeted exercises designed to reduce dizziness and improve stability through two key principles: habituation and adaptation. While performing these exercises may initially provoke mild symptoms, this controlled exposure is part of the recovery process. However, it’s essential to strike a balance—exercises should be performed at a tolerable level to avoid overexertion and worsening symptoms. In this article, we’ll explore effective vestibular exercises, guidelines for symptom management, and tips to help you optimize your recovery.
Understanding Habituation and Adaptation in Vestibular Rehabilitation
The foundation of VRT lies in two physiological principles: habituation and adaptation. Habituation focuses on reducing sensitivity to specific motion triggers. When you repeatedly expose your vestibular system to movements that provoke mild symptoms, your brain gradually learns to ignore or “tune out” the dizziness signals. Adaptation, on the other hand, is your brain’s ability to recalibrate and improve how it processes vestibular input. This occurs through repeated, controlled stimulation of the vestibular system, which encourages neural plasticity and enhances balance and coordination.
During vestibular exercises, it’s normal to experience a brief increase in dizziness—this is expected and even beneficial but needs to be performed correctly. Symptom provocation is part of the process that promotes neural adaptation. The key is keeping this symptom increase at a tolerable level and allowing time for a complete recovery for symptoms to return to baseline. Pushing too hard can overwhelm your system, while being too cautious may slow your progress.
Guidelines for Safe and Effective Vestibular Exercises
To maximize the benefits of VRT, it’s important to follow general guidelines that help monitor and control symptom intensity. A helpful rule of thumb is the 2-point rule: when performing vestibular exercises, a temporary increase of up to 2 points from your baseline dizziness level (on a 0-10 scale) before pausing and allowing full recovery. For example, if your dizziness is at a baseline of 3, an increase to 5 during exercise is acceptable. This is person specific and is meant to help determine what a tolerable symptom increase looks like for VRT.
Additionally, symptoms should fully subside within 15 minutes after you complete the exercise. If you experience more intense dizziness or require longer than 15 minutes to recover, the exercise may be too challenging. This could indicate that you need to modify the intensity, duration, or frequency. It’s also essential to tailor exercises to your individual symptom triggers. Movements that you find personally aggravating—such as quick head turns or visual motion—should be incorporated gradually and at a level you can tolerate.
Again, these are general guidelines and may not be the right fit for everyone. They may help start a conversation with a VRT provider to ensure areas being address find a balance of a challenging stimulus to provoke change while also allowing space for someone to go about the other needs and challenges of their day. Other considerations include how one’s symptoms act. If symptoms are more delayed, then a provider may recommend a lower point increase before pauses to rest to avoid a delayed symptom flare. If someone recovers from symptoms quickly, but their symptom intensity increases quickly, they may work on movements that have a slightly higher symptom point increase before pausing for recovery.
Sometimes vestibular rehab isn’t for everyone, and timing can be just as important as having appropriate exercises, more on this is discussed in this podcast.
Five Tips for Vestibular Rehab
- The 15 minute rule can act as a guide for VRT and daily activities. If symptom increases take longer than 15 minutes for return to baseline symptoms, modifying may be warranted for overall symptom management and gradual progressions exercises or pacing of daily activities.
- A general guideline on when to pause and rest can be helpful in determining the correct level of challenge while balancing time to recover. A general starting point may look like a 2 point increase from baseline symptoms. Similar to strength training, if someone isn’t familiar to resistance training, easing into reps, sets, and weight can help reduce unpleasant side effects (muscle soreness for example) to gradually increase the intensity. A similar approach for dizziness can ideally help minimize boom bust cycles.
- Exercises should be tailored to you! Make sure the plan is working towards personal goals. Similar to strength training, weights, reps and sets are designed in a routine based on the goal or outcome someone has. Incorporating aspects of activities someone wants to get back to can help encourage consistency, see the progress, and incorporate something meaningful to work towards.
- It’s okay to ask questions. Maybe your goal is to get back to trail walks, and currently you’re sitting in a chair and moving your eyes between two targets. How is that helping? The exercises you’re doing now might not look exactly as the activity you’re wanting to getting back to. Understanding the parts being worked on, and how that will progress towards your ultimate goal can be helpful in understanding the various building blocks that go into higher level activities, and how your provider is addressing those in parts to then start putting together.
- Sometimes it’s too early to start. Or there may be a need a need to pause and start later on. That’s okay and normal. Vestibular conditions can have layers, and new layers may need other ways for support to work through. Sometimes the body isn’t quite ready to take on more stress that VRT may provide (it takes stress to encourage change) and that’s not a failure. Give the body the support it needs. For example, someone with vestibular migraine may need more time to establish acute meds or a preventative med to reduce attacks before being ready for VRT.
- Incorporate fun. Use your VRT provider as a resource to return to activities that spark fun and see what ideas they have to modify. You are more than your vestibular condition. It’s important to advocate and work towards goals but it’s also important to explore the other parts of what make you you. Those that dedicate 100% of their time and effort to getting better tend to realize that when they stopped to take time for themselves, they actually saw progress faster.
Final Thoughts: Finding the Right Balance in Your Rehabilitation
Vestibular rehabilitation exercises are highly effective when performed consistently and within appropriate symptom thresholds. Mild symptom provocation is expected and necessary for adaptation, but it’s crucial to avoid pushing too far. Following the 2-point rule and ensuring symptoms resolve within 15 minutes can help you safely build tolerance and resilience. However, vestibular disorders vary significantly from person to person, and there are always exceptions. It’s essential to work with your healthcare provider or vestibular therapist to determine the best exercise plan for your specific needs. With patience, persistence, and proper guidance, VRT can help you regain stability and reduce dizziness, improving your overall quality of life.
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
How Long Does It Take to Recover from a Vestibular Disorder?
This is a frequently asked question and recovery from a vestibular disorder can depend. This post outlines considerations that play into recovery timelines for vestibular disorders. Proper diagnosis, timeliness of diagnosis and different interventions can all play in roll in how long recovery from a vestibular disorder takes. Whether caused by an inner ear infection, head injury, or a chronic condition like vestibular migraine or Meniere’s disease, recovery times vary widely. For those experiencing dizziness, vertigo, or imbalance, understanding the recovery timeline can be reassuring.
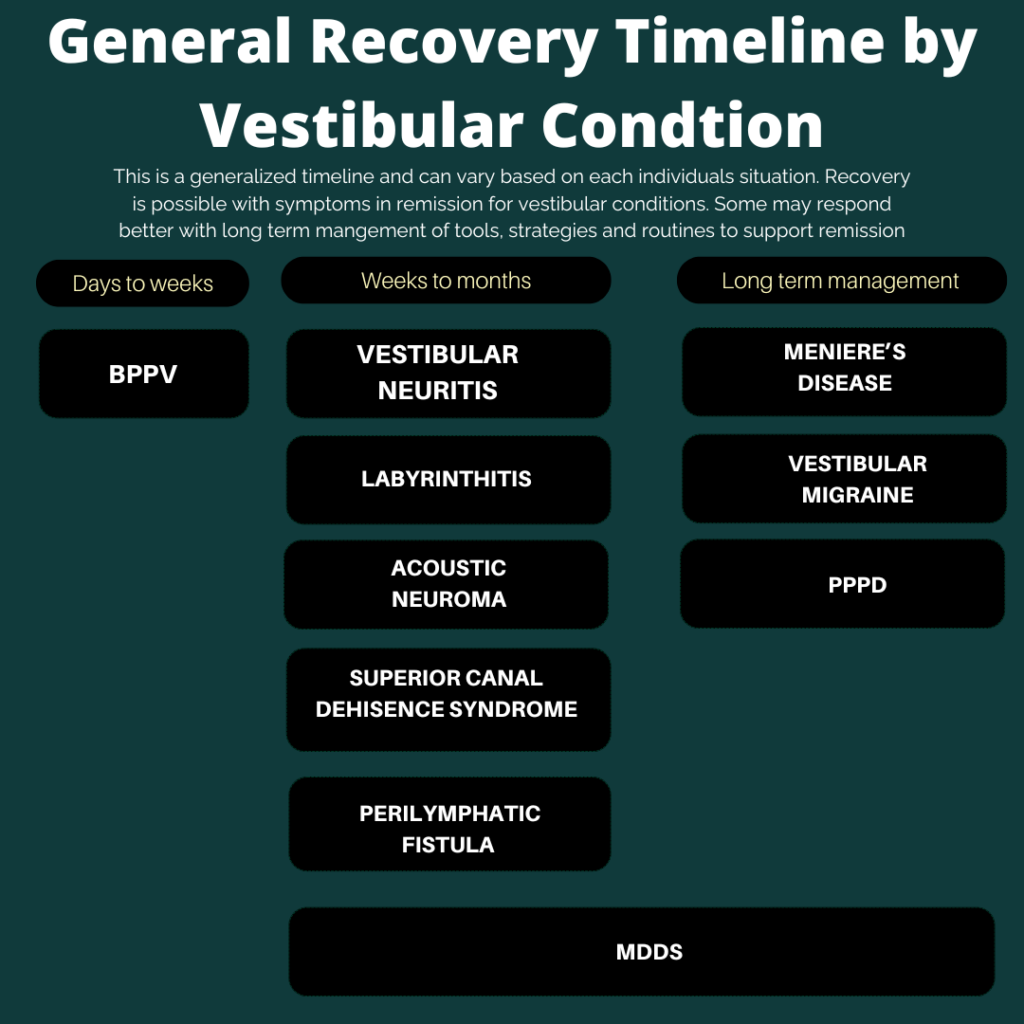
General Timeline of Recovery from a Vestibular Disorder: by condition
The time it takes to recover from a vestibular disorder varies greatly. This blog will review important considerations in determining a possible timeline to recover from a vestibular disorder.
A condition such as benign paroxysmal positional vertigo (BPPV) can be resolved in as little as one session or a few sessions. Concussion, vestibular neuritis or labyrinthitis can take weeks or months for recovery due to the nature of this condition- more time is needed as the brain adapts and habituates to the vestibular system post neuritis/labyrinthitis. Chronic vestibular disorders, such as vestibular migraines, persistent postural-perceptual dizziness (pppd) or Meniere’s disease, often require long-term management rather than a definitive recovery timeline.
In general, having a well rounded approach to health can be beneficial. When it comes to chronic vestibular disorders, having a well rounded approach is important for best management of a vestibular condition. This includes the basics (sleep, nutrition, stress management, movement), medications, mindset work, supplements and other tools and strategies as part of one’s toolkit (such as avulux glasses for light sensitivity, or ruhewell products specifically picked for dizziness) to best manage symptoms and any attacks or flare ups.
Importance of Proper Diagnosis and Care
Since vestibular disorders have varying causes and prognoses, an accurate diagnosis is crucial for effective treatment. A healthcare provider may use vestibular function tests, hearing assessments, and imaging studies to determine the underlying cause of symptoms (more on this here). Understanding and learning about vestibular conditions can be helpful in management and understanding of the timeline for recovery from a vestibular disorder. If there are multiple conditions (vestibular neuritis and vestibular migraine; or vestibular migraine and persistent postural perceptual disorder), then education can better understand how these conditions could possible impact the other, or help strategize treatment approaches.
For example, with vestibular migraine and pppd, addressing the underlying vestibular condition (vestibular migraine in this case) will overall assist with pppd. Some may focus on strategies for vestibular migraine overall, and some interventions can be beneficial for both (mindset work and nervous system regulation, possible medications for example).
Proper diagnosis is important, and timely initiation of treatment. For example, BPPV can be considered a “quick fix” with canalith repositioning maneuvers that can clear BPPV in as little as one session, but may take a couple of visits to fully resolve. If left untreated with ongoing symptoms, or delays in proper diagnosis and treatment can possibly lead to chronic dizziness such as pppd.
Timely diagnosis and treatment for vestibular migraine can assist in keeping this condition as an episodic condition (fewer than 15 days of symptoms or attacks). If delays in proper diagnosis and treatment, migraine conditions can become chronic (more than 15 days of attacks or symptoms per month). Chronic migraine conditions can become episodic again but ultimately avoiding this is ideal for overall wellbeing and management.
The Variability of Vestibular Disorder Prognosis
No two vestibular conditions are exactly alike, making prognosis difficult to generalize. Factors such as age, overall health, the severity of vestibular dysfunction, and how soon treatment is initiated all influence recovery. While some individuals recover fully within weeks, others may need ongoing management through daily lifestyle choices and tools for best long term results.
For those struggling with persistent dizziness or imbalance, patience and consistency in treatment are essential. Seeking early intervention and working closely with healthcare professionals can make a significant difference in the overall recovery process.
In Summary
Recovering from a vestibular disorder depends on the specific condition, the severity of symptoms, and the effectiveness of treatment. While some vestibular issues resolve quickly, others require long-term management and rehabilitation. Proper diagnosis and adherence to a personalized treatment plan, including vestibular rehabilitation therapy, can enhance recovery outcomes. Though the journey may be challenging, with the right approach, many individuals can regain stability and improve their quality of life.
Want to learn more about dizziness and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link here.
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Traveling with Vestibular Conditions: 5 Tips to Enjoy Your Trip
Traveling with vestibular conditions initially sounds daunting. It can be done. It can even be a trip that’s enjoyable! Proper planning and strategies can and has given vestibular warriors the tools and confidence to enjoy a fulfilling trip. This blog post explores common travel challenges for those with vestibular disorders and offers five practical tips to help you make the most of your journey.
But First, Some Proof: Successful Traveling with Vestibular Conditions
Vestibular warriors have been sharing tips, tricks, and wins on their travel adventures in Vestibular Group Fit. Here are some quick phrases that do show that travel and an enjoying your time on a trip is possible. Preparation and having tools and strategies is key. Read on to learn more how others prepare.
Anticipate Possible Challenges to Help Strategize Preparations
One reminder others have found helpful is to remember you are not alone. Thoughtful planning, coordination, and care goes into most, if not all, trips. Factoring in areas to support a vestibular condition is a new and additional consideration that does take additional time and energy when planning a trip. We are here to try and take guess work out of it. This will improve with time and experience to tailor things to best fit your needs. Having a list of travel reminders as part of packing and travel prep will help smooth out this process even further. Traveling with vestibular conditions has been done by others and can be done by you too!
Possible challenges include:
- Motion sensitivity/visual vertigo from different travel mediums (car, train, plane, boat)
- Time zone changes
- Early or late flights disrupting sleep
- Change in movement routine (travel days more stationary, maybe vacation destination with a lot of walking or other activities)
- Change in typical diet/hydration routine
- New environment (different sleeping arrangements, new noises, bright lights)
- Weather patterns or new weather conditions
- unexpected events can increase fatigue or stress
Keeping in mind possible challenges can help with prepping strategies and solutions when planning a trip and traveling with vestibular conditions. Some strategies can be utilized leading up to a trip, others will be strategies to use during travels.
A gentle reminder that traveling has its challenges for everyone and some strategies you might have done to ease these challenges can still be great tools to continue using. These sometimes inherent or universal challenges to traveling is also part of why it can be harder with a vestibular condition. This is where threshold theory can be a helpful framework. Everyone in the group challenging may be experiences the same stressors, but everyone has different thresholds as to how much those stressors will impact them.
Being kind to yourself, and prepping to best support your body and get a bigger threshold is one way to help strategize and the basis for some of the tips below. If you’re interested in more on threshold theory, check out this post here.
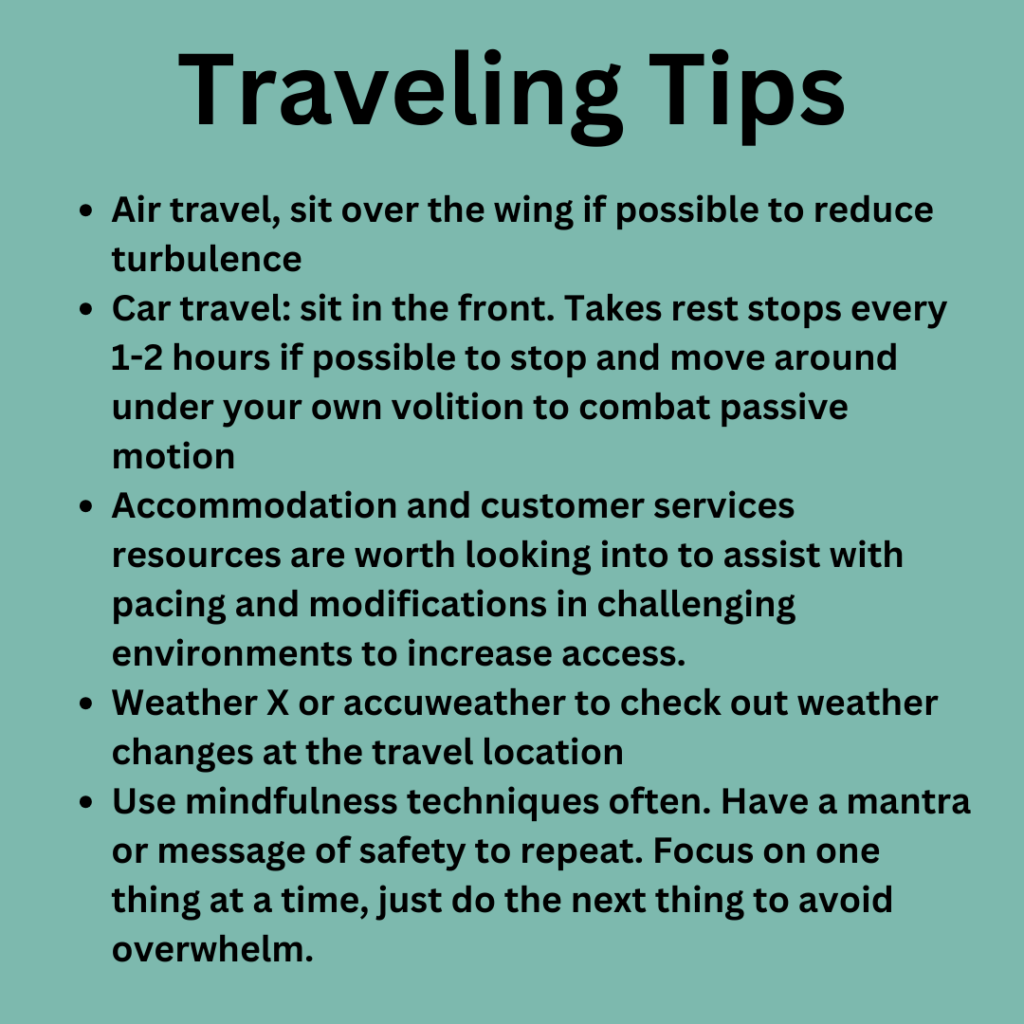
5 Tips for Traveling with Vestibular Conditions
- Stick to your routine the best you can leading up to travel. Try to incorporate supportive habits to increase your threshold and build resilience to a day of travel. Trying to stick to your typical routine the day of travel can be helpful too-modifications may be needed (lighter workout or gentle movement to conserve energy and pacing for traveling)
- Start packing early. If there are items used frequently, keep in the suitcase to avoid forgetting it. based on weather and activities, gradually pack items to avoid feeling rushed or forgetting something. Consider adding snacks for travel days to this packing list as well
- Build in rest time in your trip. Building in a rest day or low key activities the day after travel gives the body more time to adjust and gently get back into routine. Try to space out big activities throughout your trip itinerary to build in time for relaxation. During travel days, check in often to work on breathwork, mindset, meditation to pace and find calm throughout the day.
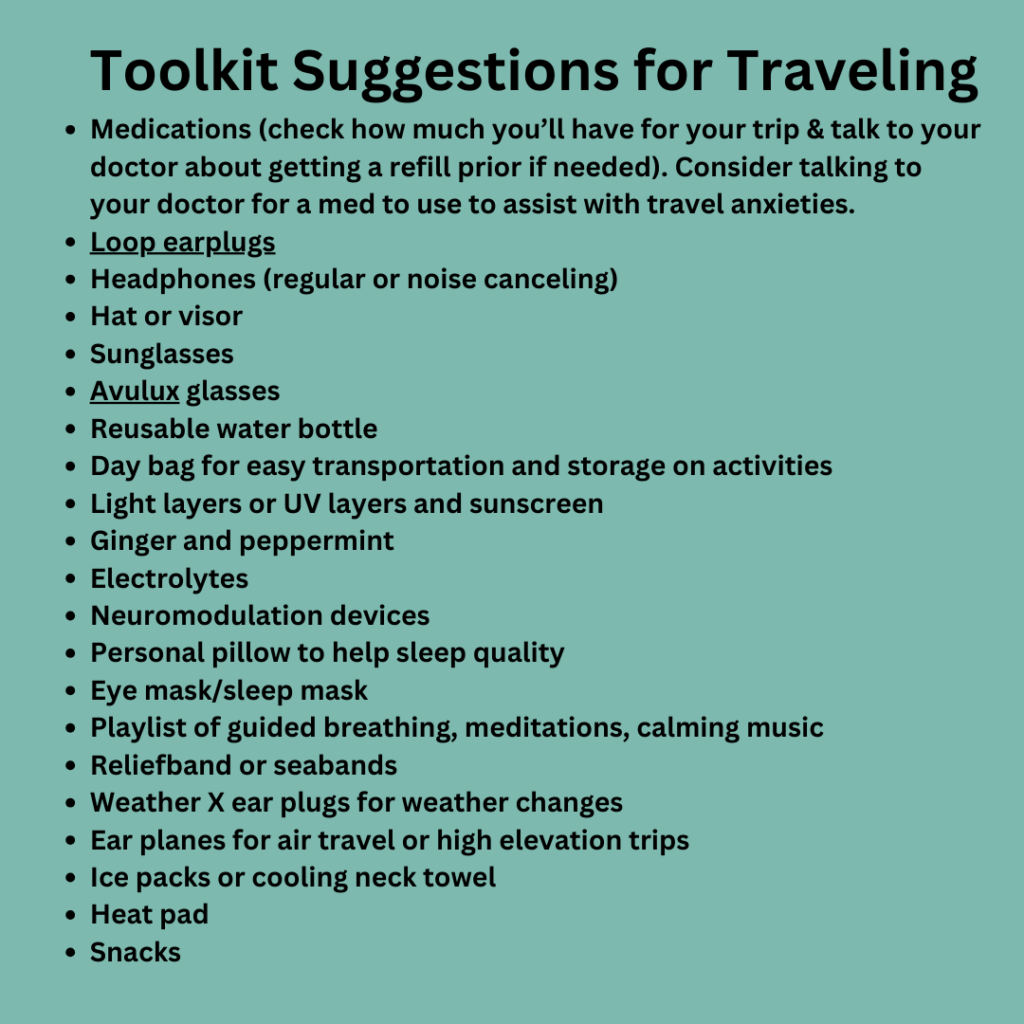
- Prep a toolkit. Have typical tools for symptoms, stopping attacks, supplements and items that help improve ones threshold packed and make sure to have enough for the entire trip. Special considerations for items based on travel and the trip as well. More suggestions below.
- Utilize accommodation services and resources. If long lines are challenging, traveling large campuses or airports that are unfamiliar, utilize resources built to help you! This can look like help getting to an airport gate, a less crowded and quite route to go through security, checking into a hotel on a lower floor to reduce elevator use or high views, or having medical clearance to bring personal snacks and water into even spaces.
- Check and see if your airport is part of the Hidden Disabilities Program
- If planning long term for an upcoming trip, consider gradually scaling mindfulness practice, balance, movement, visual and vestibular work to increase tolerance and confidence in your travels or specific travel activities.
Traveling with vestibular conditions may require extra planning and adjustments, but it doesn’t mean you have to miss out on the joy of exploring new places. By understanding your triggers, packing thoughtfully, and pacing yourself, you can create a travel experience that is both enjoyable and manageable. With the right mindset and preparation, the world is yours to discover—one step at a time. Happy travels!
Want to learn more about dizziness and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link here.
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
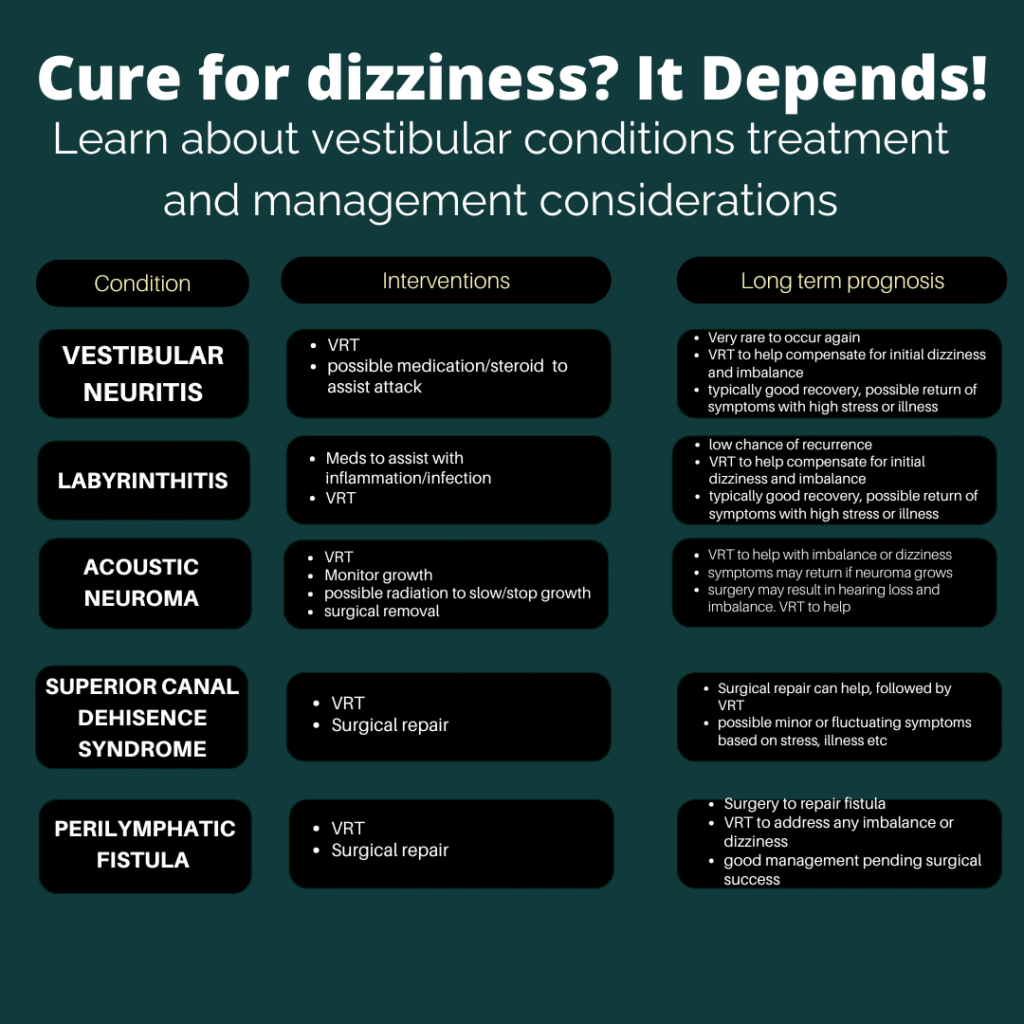
Can an ear infection make me dizzy? What is a vestibular neuritis and labyrinthitis? How are they different? In this article, we’ll delve into these conditions, explore whether an ear infection can cause them, and discuss potential treatments to help you find relief.
Both of these conditions can result in a unilateral vestibular hypofunction. Other conditions can also result in a unilateral vestibular hypofunction. This is why vestibular rehabilitation could look similar but the cause of the hypofunction may sound different between people.
The Vestibular System: Your Body’s Balance Center
Before we dive into labyrinthitis and neuritis, let’s first understand the vestibular system. This intricate network of structures within the inner ear is responsible for maintaining balance, spatial orientation, and coordinating eye movements. It consists of the semicircular canals, the utricle, and the saccule, all which have their own special role in signaling and detecting motion and gravity. Check out this blog post for further detail on vestibular anatomy in writing, or this youtube video for audio/visual presentation of vestibular anatomy.
Labyrinthitis: A Disorienting Disturbance
Labyrinthitis occurs when the labyrinth becomes inflamed. This inflammation disrupts the transmission of sensory information from the inner ear to the brain, leading to symptoms such as vertigo, nausea, vomiting, and difficulty focusing. This type of inflammation can result in hearing loss.
Vestibular Neuritis: A Nerve-Wracking Experience
Vestibular neuritis specifically refers to inflammation or infection of the vestibular nerve, often resulting from a viral infection. It typically presents with sudden, severe vertigo that can last for days to weeks, accompanied by nausea and imbalance. While the exact cause of vestibular neuritis is not always clear, it’s often associated with viral infections such as the herpes simplex virus or the varicella-zoster virus. This type of inflammation or infection does not typically result in hearing loss.
Can an Ear Infection Cause Vestibular Disorders?
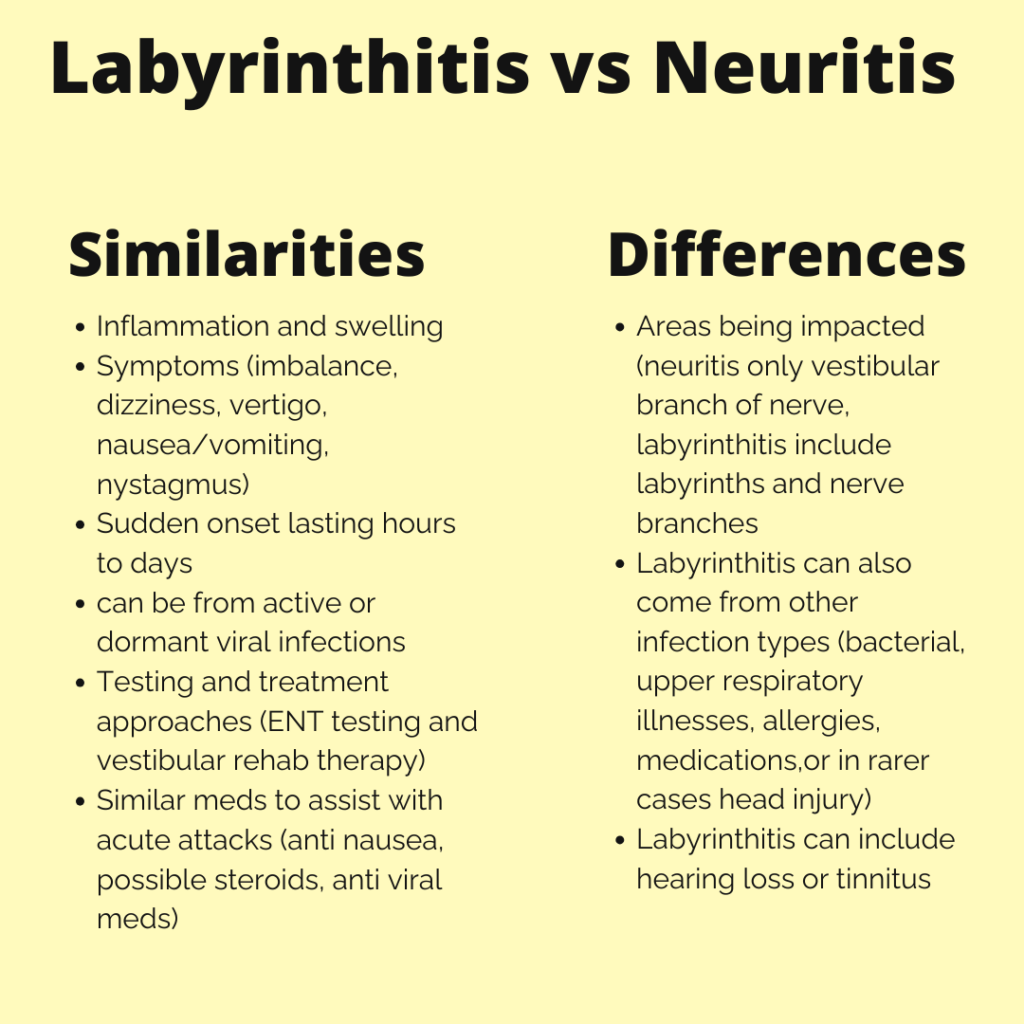
Yes, an ear infection could be a preceding event to a labyrinthitis or neuritis. The inflammation or infection itself could impact the nerve (as in the case of vestibular neuritis) or the labyrinth (in case of labyrinthitis), disrupting their normal function and causing symptoms of vertigo and imbalance. The image below outlines what structures are impacted in both labyrinthitis and neuritis to further understand the differences of these conditions.
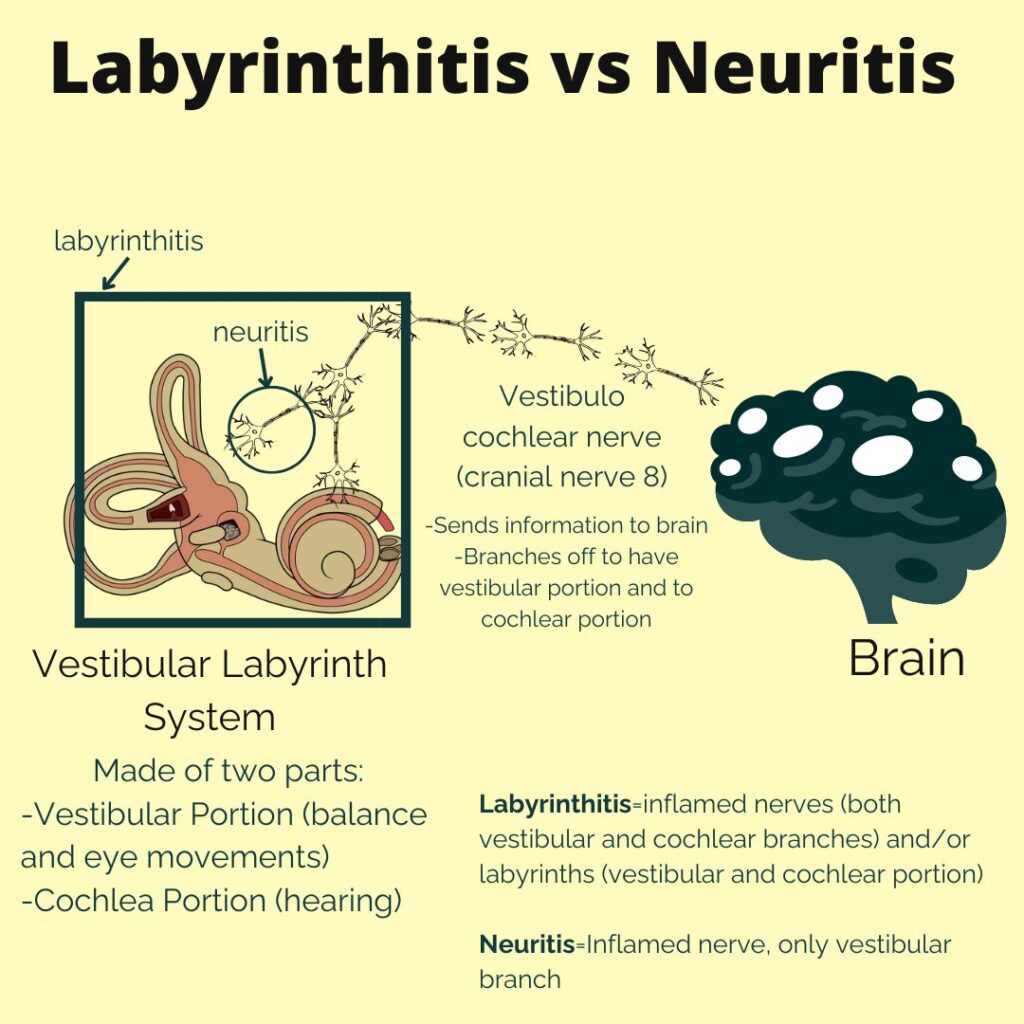
Below is a written out comparison of the similarities and differences of vestibular neuritis and labyrinthitis.
Treatments for Vestibular Disorders
If you’re experiencing symptoms of labyrinthitis or neuritis, it’s essential to seek medical attention for an accurate diagnosis and appropriate treatment. The sooner proper treatment are implemented the better. While these conditions can be distressing, there are several strategies to manage symptoms and promote recovery:
- Vestibular Rehabilitation: This specialized form of physical therapy focuses on exercises and maneuvers to improve balance, reduce dizziness, and enhance your ability to compensate for vestibular dysfunction.
- Pacing, Rest and Hydration: Adequate rest and hydration are crucial for supporting your body’s healing process and managing symptoms.
- Medications: Your doctor may prescribe medications such as vestibular suppressants or anti-nausea drugs to alleviate vertigo and nausea. This can be helpful for short term relief. While this is a tool that is encouraged to help manage symptoms, working towards adaptation and habituation through VRT is recommended for long term improvement. While medications are helpful, they can slow the adaptation and habituation process.
- Modify Challenging Activities or Environments: Minimize exposure to triggers that exacerbate your symptoms, or modify to dampen their impact. This is helpful in the present moment as a short term solution while working towards overall long term progress to these challenges.
- Address Underlying Conditions: If an underlying infection is causing your vestibular disorder, your doctor may prescribe steroids, antibiotics or antiviral medications
Conclusion: Navigating Towards Relief
Living with labyrinthitis or neuritis can feel like navigating through a dizzying maze, but with the right guidance and treatment, relief is within reach. By understanding the vestibular system, recognizing the symptoms of these disorders, and seeking appropriate medical care, you can take steps towards regaining your balance and reclaiming your life. Remember, you’re not alone on this journey, and there are resources and support available to help you every step of the way.
Want to learn more about dizziness and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link here.
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
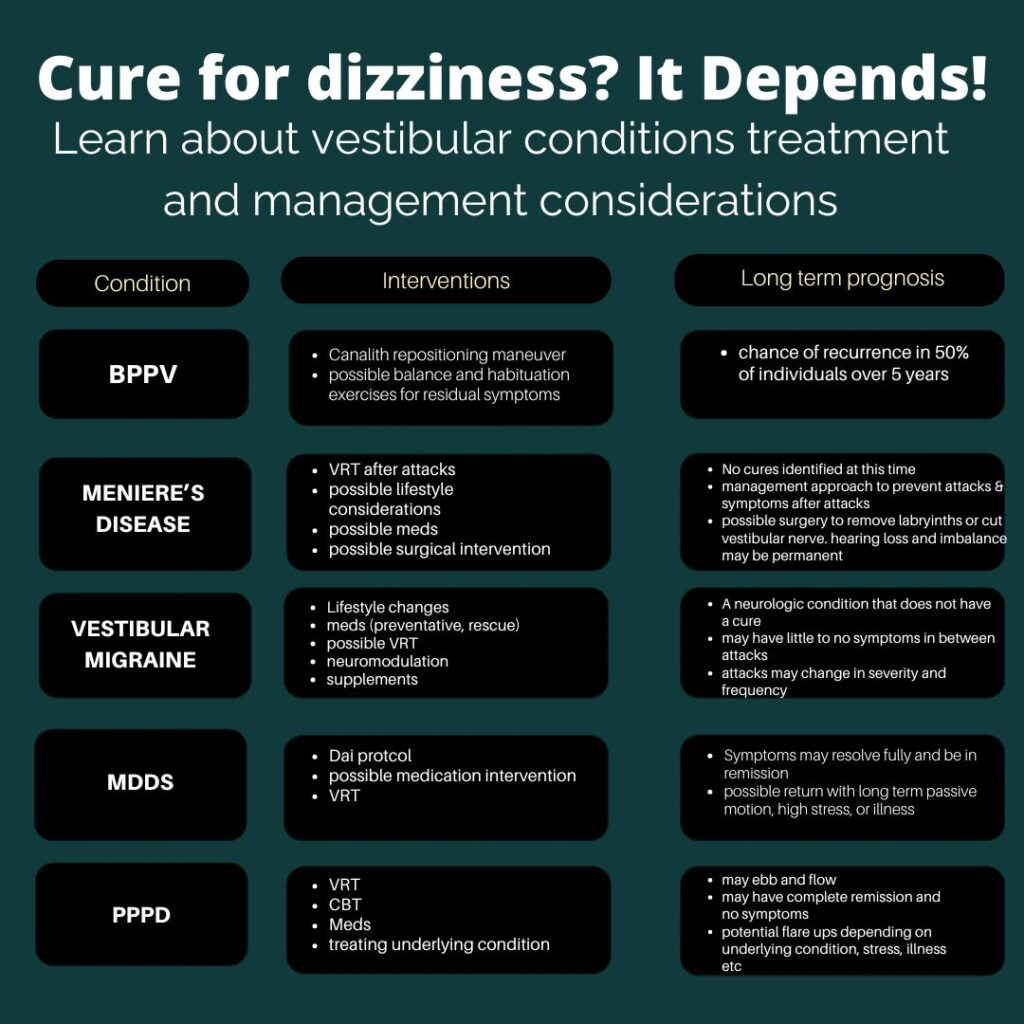
Dizziness is a common and often distressing symptom that can arise from various conditions. Among the most frequent causes of dizziness are Benign Paroxysmal Positional Vertigo (BPPV), Meniere’s disease, and vestibular migraine. While all three conditions may involve dizziness or vertigo, they have distinct underlying mechanisms, symptoms, and treatments. Understanding the differences between these disorders is key to seeking proper treatment and relief. In this post, we will explore each condition in detail and explain how to tell them apart.
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is one of the most common causes of vertigo and is often triggered by changes in head position. It occurs when small calcium crystals, called otoconia, dislodge from their usual location in the inner ear and migrate into the semicircular canals, disrupting the normal flow of fluid. This disturbance causes sudden, brief episodes of vertigo, particularly when turning the head, lying down, or getting up. Symptoms of BPPV include spinning sensations, nausea, and balance issues, but hearing loss or headaches are uncommon. Fortunately, BPPV is treatable through repositioning maneuvers, such as the Epley maneuver, which helps return the crystals to their proper place, alleviating symptoms.
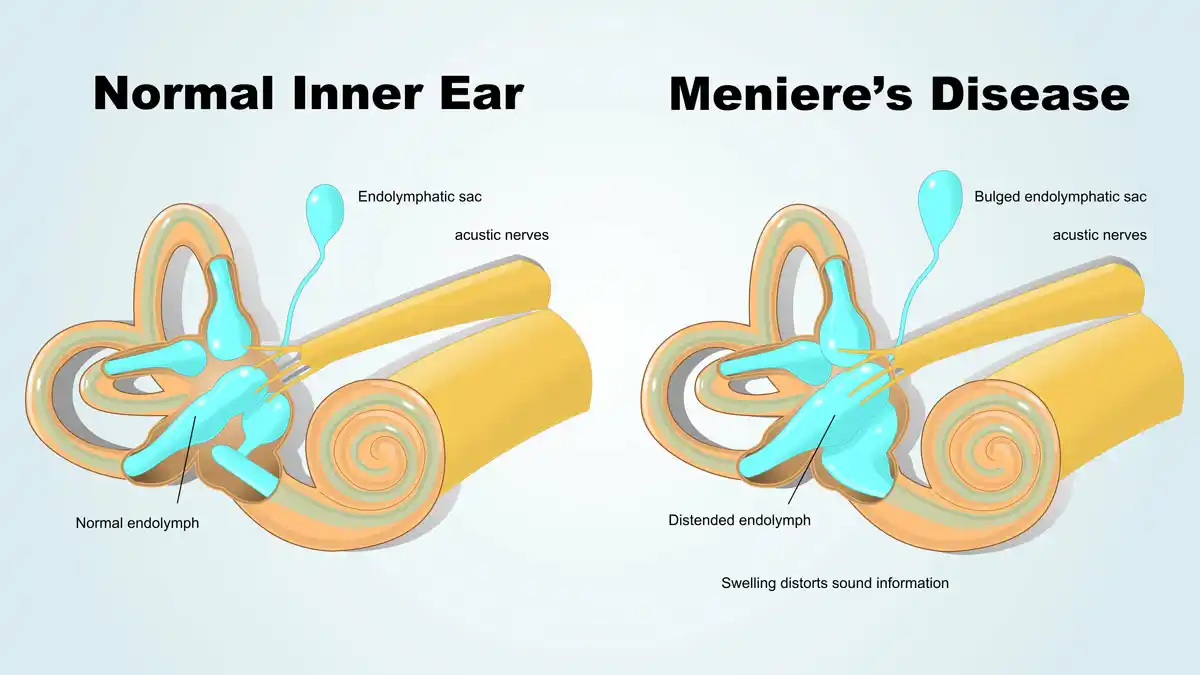
Meniere’s Disease
Meniere’s disease is a chronic inner ear disorder characterized by episodes of vertigo, fluctuating hearing loss, tinnitus (ringing in the ear), and a feeling of fullness in the affected ear. The exact cause of Meniere’s is not well understood, but it is believed to result from an abnormal amount of fluid (endolymph) in the inner ear. Vertigo attacks in Meniere’s disease can last anywhere from 20 minutes to several hours and are often accompanied by severe nausea and vomiting. Hearing loss may become permanent over time, and the condition typically affects one ear. Treatment focuses on managing symptoms through medications like diuretics, a low-sodium diet, and in some cases, vestibular rehabilitation or surgery for severe cases.
Vestibular Migraine
Vestibular migraine is a type of migraine that primarily affects the balance system, causing dizziness or vertigo without the classic headache. People with vestibular migraines may experience episodes of dizziness lasting from a few minutes to several hours, often accompanied by sensitivity to light and sound, visual disturbances, nausea, and sometimes mild headache. Unlike BPPV or Meniere’s disease, vestibular migraine is rooted in abnormal brain activity affecting the vestibular system. Treatment involves a combination of migraine management techniques, including dietary and lifestyle changes, medications to prevent migraines, and vestibular rehabilitation exercises to improve balance.
Similarities and Differences
While BPPV, Meniere’s disease, and vestibular migraine all involve dizziness or vertigo, they differ significantly in their causes and associated symptoms. BPPV is characterized by short, triggered episodes of vertigo linked to head movements, whereas Meniere’s disease presents with longer-lasting vertigo episodes, hearing loss, and ear-related symptoms. Vestibular migraine, on the other hand, can mimic both conditions in terms of dizziness but is usually linked to migraine symptoms like visual aura or light sensitivity, without ear-related issues. The duration and frequency of vertigo attacks, as well as the presence of other symptoms like hearing loss or migraine, are crucial in distinguishing between these conditions.

Summary
Differentiating between BPPV, Meniere’s disease, and vestibular migraine is important for proper diagnosis and treatment. While BPPV is related to mechanical issues in the ear, Meniere’s disease involves fluid imbalances, and vestibular migraines are linked to brain activity. Each condition has unique symptoms and treatment approaches, but understanding the key differences can help those suffering from dizziness seek the most appropriate care and manage their condition effectively. If you are experiencing unexplained dizziness, a visit to a healthcare provider specializing in balance disorders can help determine the cause and provide the necessary treatment plan.
Want to learn more about dizziness and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://thevertigodoctor.com/vestibular-group-fit
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
What is the Best Treatment for BPPV?
Benign Paroxysmal Positional Vertigo (BPPV) is a common cause of vertigo, characterized by brief episodes of dizziness triggered by changes in head position. This condition occurs when tiny calcium particles (otoconia) in the inner ear become dislodged and enter one of the semicircular canals, leading to a sensation of spinning.
BPPV Background and Anatomy
Otoconia are calcium carbonate crystals that reside in the utricle and saccule. The utricle and saccule help detect linear motion (up/down, forward/backward, side to side, tilting). The otoconia assist in this by responding to gravity which sends signals to the brain to interpret motion. Imagine a jar full of pebbles, tilting the jar will cause the pebbles to change distribution. The brain can take information like this and understand which direction the head is tilting, and direction of movement.
The semicircular canals are filled with a fluid called endolymph, and the job of the semicircular canals is to sense rotational movement. There are three canals positioned in different angles to detect different types of motion. As the fluid (endolymph) moves at various speeds in the different canals, tiny hair like cells called cilia move, and the brain is able to determine direction of movement and change in speed of movement. So what happens when a otoconia crystal winds up in the endolymph fluid of a semi circular canal? BPPV
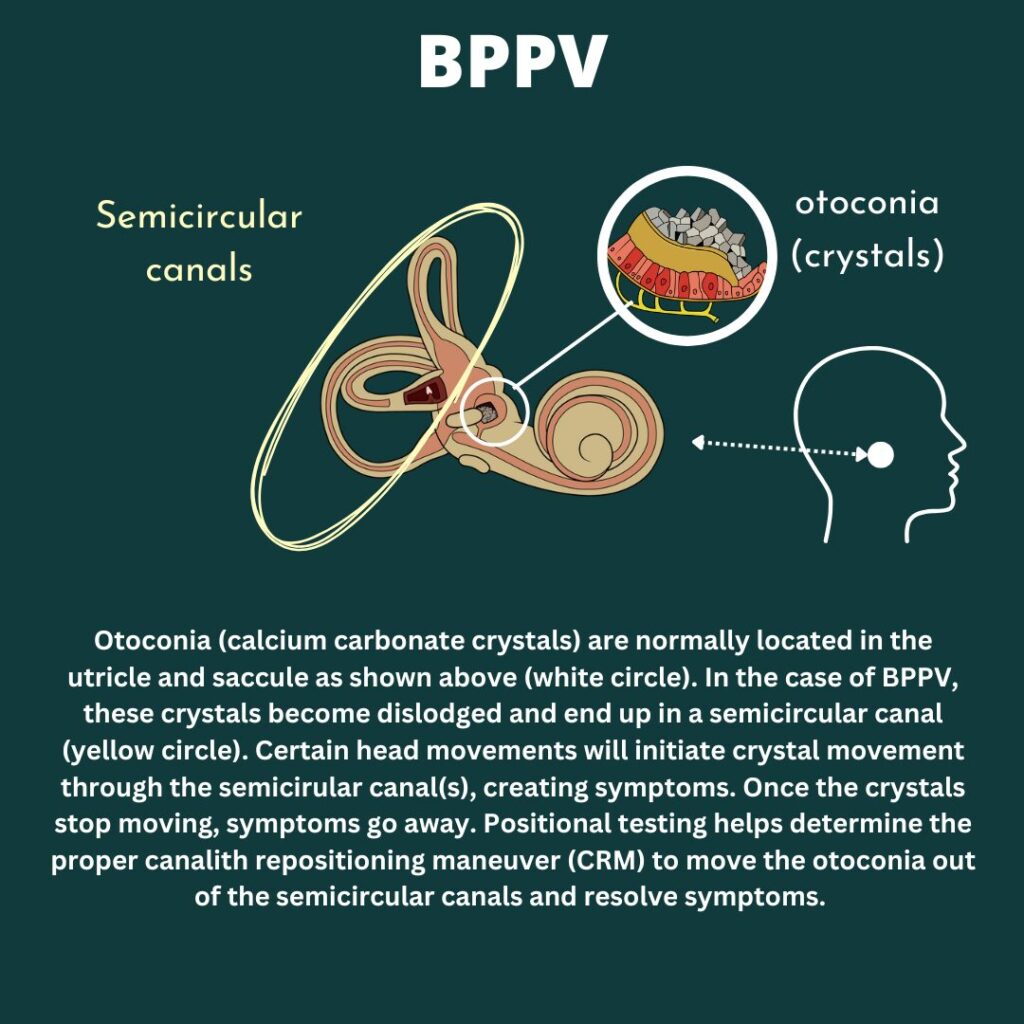
BPPV results in short, intense sensation of room spinning. This is brought on typically with certain head or body positions. As a provoking head position is brought on, the otoconia/crystals are encouraged to start moving due to gravity’s pull. As the otoconia move through the canal, this changes the rate the endolymph moves in the affected canal(s). This results in the brain getting mismatched signals from the vestibular systems and symptoms of dizziness, unsteadiness, room spinning, nausea, anxiety, sweats etc.
Vestibular information tells the brain movement information to help with balance and knowing where the body is in space. This information also helps the brain direct the eyes in the same direction and speed of the body for smooth gaze (vestibulo-occular reflex). With BPPV, the brain is getting multiple signals and is trying to have the eyes follow, resulting in nystagmus. Nystagmus is an involuntary, rhythmic eye movement. This can happen for other reasons, and can occur in different directions. This is helpful when testing, diagnosing and treating BPPV.
Assessing BPPV
Assessment for BPPV involves positional testing. This includes head and body movements while assessing for symptoms and any eye nystagmus. Each portion of the assessment is important in an accurate BPPV diagnosis and determining the correct maneuver to treat the involved canal(s). Positional testing assessing each canal. Determining which position recreates what someone has been feeling, and noting the direction of nystagmus helps determine which canal(s) and which side (left or right) is involved. This guides proper set up and treatment for BPPV.
Treatment for BPPV
Canalith repositioning maneuver (CRM) is commonly used to treat BPPV. It is important to properly assess the correct side and canal involved to choose and set up the correct CRM. The goal of CRM is to have otoconia travel through the semicircular canal and fully clear out of the canal to resolve symptoms. The Epley maneuver is a very common and successful treatment for posterior canal BPPV. If another canal is involved, other maneuvers is needed. A vestibular physical therapist can assess and determine next steps. Other providers that may address this can include ENTs or chiropractors but on an individual basis.
There are no medications that treat BPPV. There are some medications that can be helpful during treatment to better tolerate any dizziness or nausea. In rare instances, surgery can be performed to plug the posterior semicircular canal. This includes it’s own risk such as hearing loss and best to be discussed with a medical professional.
There are ways to treat BPPV at home. Assessment is still important to determine if symptoms are in fact BPPV and identifying the proper maneuver to set up. Some people have the same side and canal each time and will be taught at home CRM by their provider that they have seen for BPPV treatment. If recurrence is few and far between, or can involve different canals, the healing vertigo app is a great resource when at home, out of town, or needing guidance on positional testing and determining the proper home set up.
Guidelines for BPPV Treament
Typically, I recommend 2-3 maneuvers in a session and then give a day or two to see what’s improved. It’s normal to feel “off” or worse after a treatment session and then feel overall better once given some time to recover. Sometimes people feel immediately better after a session, other’s don’t, and they both be cleared of BPPV. Allowing 1-2 days post treatment can get a better idea how one is really feeling after allowing the body time to recover after treatments. Treatment does recreate dizziness in order to move the otolith through the canal, and why people can feel worse after, and why medications can help make treatments more tolerable. This is just a starting point and can be adjusted based on the person. Sometimes I’ve done one maneuver, other times five or more, it just all depends!
Some recommend avoiding certain movements, this is okay to a point, but avoiding movement forever or being afraid to move is not the end goal. Taking a day to avoid larger bending or laying flat is okay for comfort, but getting back into basic routine will ultimately give the feedback needed to determine if more treatment or assessment is needed.
Sometimes BPPV is cleared and certain movements can feel “off” as the body adjusts to vestibular systems with cleared BPPV. Some vestibular rehabilitation therapy and balance work can help after BPPV treatment and clearance to help any lingering or residual sensations.
Want to learn more about BPPV treatment and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://thevertigodoctor.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Dizziness triggers: threshold theory and 10 contributors to dizziness
Many are on the hunt for dizziness triggers. “What is the one or two things that make my dizziness worse”. “If I just figured out my trigger I can get rid of it and not be dizzy anymore”. The many variables in day to day life, both within and outside our own control, makes this a futile effort. This leads to feeling overwhelmed, hopeless, frustrated, and depleted. This article will discuss a different approach known as threshold or bucket theory as well as considerations of what may contribute to one’s threshold. We’ll also cover ways to track this and create a bigger threshold for long term growth and management.
What is threshold (bucket) theory? Why is this better than finding specific dizziness triggers?
Finding specific dizziness triggers or the root cause to dizziness sounds great in theory but much harder in practice. Each day is different, making this hard to track. There might be areas that might contribute to dizziness but is outside anyone’s control (weather, infection, allergies) so then what?
Threshold or Bucket Theory helps account for the variability of life, things within our control and outside our control, and why it’s rarely just one thing. Think of a bucket, and dizziness triggers fill up the bucket. Different things may fill up the bucket more or less on different days. On better days we might have a bigger bucket, on less ideal days the bucket is smaller. When the bucket starts to reach full capacity or even starts to overflow, symptoms are heightened or even a full on attack.
Looking at what may contribute to ones bucket can help strategize and know what days may be more challenging and more support is needed, see what is within our own control to be modified, finding grace for things outside ones control, and working on growing a bigger bucket.

Contributors to threshold (or possible dizziness triggers depending on the day)
The picture above illustrates threshold theory and common “dizziness triggers” or contributors to ones threshold. This better shows how it’s rarely one thing that sets off a dizziness flare or attack and more likely a combination of factors, including a lower threshold/smaller bucket. Listed below are common contributors, and we’ll go into a bit more detail in the next section.
- Stress
- Poor Sleep
- Poor Hydration
- Hormones
- Weather Changes
- Illness/Sickness
- Dizzy Anxious Cycle
- Environment
- Seasonal Allergies
- Muscle tightness/Lack of MovementLet’s dive deeper into each of these topics below!
- Stress: High levels of stress can exacerbate vestibular symptoms by triggering physiological responses like the fight or flight response. Stress can tie into the dizzy anxious cycle but can be it’s own separate contributor as well. Chronic stress can lower ones threshold can lead to other health impacts such as poor sleep, muscle tension, headaches, high blood pressure and more.
2. Poor Sleep: Inadequate or poor-quality sleep can disrupt the body’s natural rhythms and impair cognitive function and processes that help with memory and learning. Learning is an area that’s important when healing and recovering from vestibular conditions as part of positive neuroplasticity. Learning and brain function help with reweighing of the sensory systems (why Vestibular therapy works!) Sleep deprivation can lower ones threshold by making it harder for the brain to carryout tasks. With a vestibular condition, the brain is working harder to determine spatial orientation and movements, and trying to determine the correct response. When functions require more resources, sleep is important to optimize function.
3. Poor Hydration: Dehydration can disrupt the balance of fluids and electrolytes in the body, affecting blood pressure and circulation. This may be important in certain populations such as those with POTs (Postural Orthostatic Tachycardia Syndrome). Being properly hydrated is again important to best support the body for healing and recovery.
4. Hormones: Fluctuations in hormone levels, such as those experienced during menstruation, pregnancy, or menopause, can influence vestibular function and trigger dizziness. There are some blog posts that go into more detail on the website. But there’s some amazing in depth information and discussions for Vestibular Group Fit Members.
5.Weather changes: Variations in barometric pressure, temperature, and humidity can contribute to ones threshold. Think of weather as a possible stressor to the body. Sudden changes in weather conditions may lower the threshold for dizziness and vertigo, especially for individuals with sensitivity to atmospheric pressure changes. The weatherx app and ear plugs can better assist tracking possible connections to barometric pressure shifts, and weather x ear plugs to assist in minimizing the impact of the weather.
6. Illness/Sickness: Viral infections, bacterial illnesses, and other health conditions can add stress to the body. As the body is fighting off an infection, energy and resources are being diverted to fight off an illness. Illness-related symptoms may lower the threshold for experiencing vestibular symptoms, particularly during periods of acute illness or recovery.
7. Dizzy-Anxious cycle: The relationship between dizziness and anxiety can create a vicious cycle where dizziness triggers anxiety, and anxiety exacerbates dizziness symptoms. This cycle can quickly fill ones threshold. This cycle can be broken, and why mindfulness and mindset work is so so important. Consider a professional to assist with tools and coping strategies. A whole section on medications, breathwork, and tools are in Vestibular Group Fit for members to explore.
8. Environment: Environmental factors such as noise, lighting, and visual stimuli can worsen dizziness. Certain environments, such as crowded or visually stimulating spaces, may lower ones threshold as well if visual vertigo or motion sensitivity is part of ones vestibular condition (hint: it is for many).
9. Seasonal allergies: Allergic reactions to pollen, dust, or other environmental allergens can exacerbate inflammation and congestion in the sinuses and even feel like plugged ears. Seasonal allergies may lower the threshold for experiencing dizziness and vertigo, especially during peak allergy seasons, everyone responds to allergies different, but springtime can be tough for vestibular warriors between weather shifts and pollen counts.
10. Muscle tightness/Lack of movement: Muscle tightness, especially in the might back, upper trap and neck region can impact migraine conditions and dizziness. Muscle tightness and resulting pain or a state of discomfort can make other symptoms worse as well. The body likes to move, and having tight, stiff, painful muscles or a fear of movement from dizziness and unsteadiness can become a vicious cycle.
How to track dizziness triggers or your threshold contributors
Using apps like Migraine Buddy or keeping a symptom journal can be valuable tools for tracking possible dizziness triggers in individuals with vestibular disorders. However, it’s important to approach symptom tracking mindfully to avoid hyperfocus, which can exacerbate symptoms and diminish quality of life. Rather than constantly monitoring, it’s recommended to track symptoms after noticing an increase or flare in dizziness.
Record information from the past 1-2 days, things like:
- hormonal fluctuations.
- stress levels
- weather
- allergies
- meals (skipped meals, different meal times, missed a bedtime snack, less nutrient dense meal etc)
- sleep
If experiencing increased symptoms or a flare, consider tracking symptoms leading up to the event, any medications taken, and strategies employed for relief. This can help identify patterns or prodromal signs preceding an attack and evaluate the effectiveness of medications or interventions. Remember, the goal is not to obsessively monitor every moment, but to gather insightful data that can inform targeted interventions and improve symptom management over time.
How to get a bigger threshold
Growing a larger threshold over time to better manage vestibular disorder symptoms involves a holistic approach that encompasses various aspects of health and well-being. Luckily, some of these are little to no cost, no doctors prescription needed. Building a bigger bucket does require consistent routine changes. Start small start slow. Build up a new routine one thing at a time, then add another. Check out a podcast on this here.
Just a reminder as well, certain factors like allergies, weather fluctuations, or illness may be beyond our control. Focusing on strategies within our control can help grow a larger threshold over time, allowing us to better absorb dizziness triggers we cannot control. There are some tools to try such as Weather X ear plugs before barometric pressure shift, allergy medication or natural nasal spray, measures to reduce risk of illness during cold and flu season. These may be good and useful tools to implement based on the situation.
Ways to grow a bigger bucket:
- Consistent, high-quality sleep is fundamental, as it supports overall health and resilience to stress.
- Regular movement, tailored to individual capabilities, promotes physical strength and balance, while staying adequately hydrated ensures optimal functioning of bodily systems.
- Engaging in mindset work and stress management techniques can help cultivate resilience and reduce the impact of stressors on symptoms.
- Environmental changes/workplace accomodations such as blue light glasses like avulux, blue light filters for computer use like iris tech, light covers for overhead fluorescent lighting, loop ear plugs etc.
- Seeking assistance from healthcare providers and building a supportive provider team can offer valuable guidance and resources for symptom management.

Living with a vestibular disorder requires patience, resilience, and a proactive approach to managing triggers and symptoms. By incorporating lifestyle modifications, stress management techniques, and awareness of your personal threshold, you can take control of your condition and improve your overall well-being. Remember, you’re not alone in this journey, and seeking support from healthcare professionals and fellow individuals living with vestibular disorders can provide valuable guidance and encouragement. Together, we can navigate the challenges of dizziness and find moments of stability and balance in our lives.
Disclaimer
Want to learn more about threshold contributors, tools to manage contributors, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
7 Ways to find support for vestibular conditions
Having support for vestibular conditions in various aspects of life are essential for navigating this challenging journey. Vestibular conditions truly take a village of friends, family, providers, and professionals to help along the path to confident management. In this blog post, we’ll explore various avenues for seeking support and connecting with others who understand what you’re going through.
7 areas to find support for vestibular conditions
- Support Groups
- Counseling
- Return to Work Accommodations
- Medical Intervention
- Holistic Intervention
- Friends and Family
- Success Stories
1. Support for vestibular conditions: Support groups
In today’s digital age, online communities have become invaluable sources of support and solidarity. Platforms like Facebook groups, Reddit communities, and online forums host discussions where individuals share experiences, coping strategies, and encouragement. Joining these groups can provide a sense of belonging and reassurance that you’re not alone in your journey. There are some great vestibular warriors and providers that help host local and online support groups. Here’s some resources on finding one to join.
2. Support for vestibular conditions:
Counseling
Living with a vestibular condition can take a toll on your mental health, leading to feelings of anxiety, depression, or isolation. Seeking counseling or therapy can be immensely beneficial in navigating these emotional challenges. A professional can help provide a safe space to vent and work through challenging emotions and grieving that is so normal to arise. It can be hard to find a professional that knows both counseling and vestibular conditions. One provider that does is Dr. Emily Kostelnik (The Vestibular Psychologist) Who is a licensed clinical health psychologist and fellow vestibular warrior. Her and her team of mindset coaches are great to work with. Other options for support for vestibular conditions include a therapist that has background in chronic pain. Chronic pain can have similar overlap to chronic dizziness. Finding a provider can be done through different databases. Feel free to check out here & here. It can take some time to find a counselor that really clicks; it’s okay to switch therapists!
3. Support for vestibular conditions: Return to work accommodations
Vestibular conditions make most, if not all, jobs challenging to complete. This does not mean returning to the same job can never happen. People have returned to work. This can look like a gradual return to work program and/or requesting reasonable accommodations to support job tasks. Going part time and building up hours, blocking off certain parts of the day to space out challenging tasks, requesting an office location that is quiet, remote work etc. More on this in a blog post here. The Job Accommodation Network is a great resource as well to learn what accommodations are common with dizziness, and prompts to help determine what may be requested based on specific job tasks. Return to work can include a combination of other interventions as well as modifications to best give support for vestibular conditions.
4. Support for Vestibular Conditions: Medical intervention
Navigating the medical side of vestibular conditions can be murky. Understanding how the vestibular system works (video here). Can turn fear into empowerment. Understanding which providers can be helpful or finding ones to team up and help create a management plan can help give the body the support needed to recover. Navigating specialists, tests, and various treatment routes can be hard to do alone. Having resources and community from others who have experienced this can help.
5. Support for Vestibular Conditions: Holistic intervention
Holistic work has its own seat at the table. Meditation, mindfulness, tai chi, yoga, herbs, supplements, guided visualization are different ways a holistic approach can be incorporated. Finding calm and safety is important for taming the dizzy anxious cycle and rewiring movements to mean safety. Finding self compassion and acceptance is huge here as well.
6. Support for Vestibular Conditions: Friends and family
Finally, don’t underestimate the power of building a personal support network comprised of friends, family, and loved ones. Communicate openly with those close to you about your condition, how it impacts your life, and what support you need. Their understanding and empathy can provide a strong foundation of support as you navigate the ups and downs of living with a vestibular disorder. This can be challenging and something talked about in detail within small group coaching and Vestibular Group Fit. Check out this episode that discusses dating, or this blog.
7. Support for vestibular conditions: Success stories
Knowing you aren’t alone is a huge weight off ones shoulders. But what about next steps? Or hope for the future? Hearing others journeys and successes is an uplifting reminder that you aren’t alone and it does get better. Here are some written options, and more with audio at Grounded: The vestibular podcast
Vestibular Group Fit
All this and more can be found in Vestibular Group Fit. This low cost monthly subscription has education, community, support and guidance to answer your questions and find your path to healing and management. Learn about the ‘why’ here.

Disclaimer
Want to learn more about strategies, information, tools and support for vestibular conditions? Get vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
5 Habits to Help vertigo and dizziness: A guide towards relief
Vertigo and dizziness can be disorienting, isolating, frustrating, and challenging to navigate. Learn how to help vertigo and dizziness in daily habits. In this article you’ll find information on daily habits that can assist in management of dizziness, and strategies that are discussed in detail with subscription to Vestibular Group Fit. There will be some discussion on other routes to compliment these habits but this list is not exhaustive. This list is designed to show common habits that have helped others, and can be relatively low cost or free to instill, with no prescription from a doctor needed.
5 Habits to help vertigo and dizziness
- Hydration. Many many people are not properly hydrated. Ensuring proper hydration is a daily habit that can better support the body and vestibular system. Many find adding electrolytes to help their hydration has assisted with brain fog, dizziness, energy etc. Talk to your doctor before adding electrolytes to your diet
- Stress and Mindset Management. One of the largest contributors to migraine attacks is stress (the other poor sleep we’ll talk about later). Stress can act like gasoline on the smallest of embers to really light up a fire. Being able to have coping mechanisms to address stress, as well as tools to modify or adjust stressors that are within control is important for overall quality of life as well as vestibular, vertigo and dizziness management.
- Nutrition. Sometimes diet changes such as limiting alcohol or caffeine intake can be helpful. This can also help anxiety and sleep quality. Adding healthy fruits and vegetables to have a well balanced diet to include protein, carbs and fats is helpful for stabilizing blood sugar and can help with overall health but also dizziness. Protein and well balanced meals and snacks have helped others reduce or eliminate later afternoon crashes, middle of the night or morning attacks. Making dietary changes should be discussed with your doctor prior to making changes, and consider a professional nutritionist or dietician for further assist and guidance.
- Movement. The body craves movement. The vestibular system helps measure movements and the brain takes those signals to make any adjustments to stay safe. Movement helps with strengthening the connection between vestibular system and the brain. Movement helps with stress, anxiety, improved sleep, improved health, hormones and so much more. This is a pillar of Vestibular Group Fit and is important to start small and gradually progress. Slow and steady. Gentle movement such as a short walk, gentle yoga or tai chi. Beginner workouts or dance classes are all great options (and also included with modifications and considerations for vestibular conditions in Vestibular Group Fit) Discussing with your doctor before performing a new exercise program is encouraged.
- Sleep. Quality, consistent sleep helps healing and giving the brain and body the rest it needs to learn, rewire and heal. Consistent sleep wake times, even on the weekends, setting up a bedtime routine, and getting quality sleep is again, important for general health but also long term management of vertigo and dizziness.
- Switch to natural options when possible. Switching to natural cleaners, soaps and detergents can take possible irritants out of the home. Brands like Branch Basics help make this easy!

Other considerations to help vertigo and dizziness
The habits mentioned above can be great to help vertigo and dizziness. Some notice considerable change when changing habits, others notice the benefits after staying consistent for 3-4 months. Others notice this has helped support other treatments to feel their best.
Other treatments, providers, or interventions may be needed for the right resources, or to help get the body to a place where daily habits can act as a considerable part of management.
This may look like medications to help break the dizzy anxious cycle, vestibular rehab therapy to scale movements back to daily routines, vision therapy to address visual symptoms, neuro modulation devices, Botox injections, and having medications to prevent or stop attacks from starting.
This can look different to everyone as everyone’s situation and background is unique to them which is why this list is not exhaustive but mean to highlight common habits that help. More resources, information and recommendations exist in Vestibular Group Fit by both expert vestibular practitioners and other vestibular warriors with their own knowledge, experience, and support.
Living with vertigo and dizziness can be challenging, but it’s essential to remember that relief is possible. By incorporating these practical tips into your daily routine, you can better manage your symptoms and regain control over your life. Remember to consult with a healthcare professional if your symptoms persist or worsen, as they can provide personalized guidance and support on your journey toward wellness.
Disclaimer
Want to learn more about daily habits to help vertigo and dizziness as well as other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Managing Anxiety and Stress to Help Dizziness
Your head spins, the room seems to sway, and suddenly, your heart races. If you’ve ever felt this, you’re not alone. Anxiety and stress can make dizziness worse. However, understanding the connection between anxiety and dizziness and learning coping strategies can greatly alleviate its impact on your daily life.
Overview: Dizzy Anxious Cycle
The dizzy anxious cycle is so important in learning about and addressing for best results and management. This can be a ‘chicken or the egg’ scenario, but dizziness can bring on anxiety, anxiety can make dizziness worse, worsening dizziness makes anxiety worsen and on and on this cycle can spiral. Working on breaking this cycle can be a game changer for dizziness. This can be done a variety of ways and different professionals to assist. More on the dizzy anxious cycle in a blog here, or podcast here.

Overview: Dizziness and Stress
Stress has a tendency to act like gasoline on a fire. Now there is such a thing as good stress. Lifting weights or running faster/longer distances are technically stress to the body, but helps promote adaptations and progress in a way that benefits the body long term when done correctly. Good or bad, stress can take a toll on the body, especially when the body is under more stress than it can tolerate.
Dizziness and worsening symptoms adds stress to the body, making it hard to tolerate other stressors. Some stress we can be in control of, other times source of stressors are outside our control. Learning how to manage stress, especially stress outside our control, is important part of dizziness progress and management. Learning how to react to stress creates a ripple effect through emotions, attitude/mindset, and actions.
Overview: Depression and Grieving with Dizziness
While taking time to talk about anxiety and stress, depression or grief may be mixed in with these other emotions. Dizziness can be accompanied with feelings of depression, loss, and mourning of “life before dizziness”. These feelings are valid and real and should be processed in order to find coping strategies and work towards growth. This may need to be done with professional guidance. Check out this website to help find a mental health therapist to work with.
Managing Anxiety and Stress
Thankfully, there are effective coping strategies to manage anxiety and stress. Drawing insights from the Anxiety and Depression Association of America (ADAA), as well as anecdotal advice from other vestibular warriors and vestibular therapists, here are some practical tips to regain control:
- Breathwork
- Grounding
- Mindfulness
- Movement/Exercise
- The Basics
- Professional Help (linked here is another source to help find professional help)
We’ll get into the specifics below with examples of each.
1.Breathwork: There are a variety of breathing techniques that can help with relaxation. The goal of these techniques is to tap into the “rest and digest” part of our nervous system and help turn off the fight or flight system. Finding what works best for you is the goal. Deep, slow breaths is the goal.
Some examples are: yoga breathing, box breathing, triangle breathing, alternating nostril breathing, physiologic sigh etc.
2. Grounding Grounding is aimed to help anchor you to the present moment. This is helpful when not feeling connected to ones body and feeling disassociated.
Try the 5-4-3-2-1 method: identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste.
Another example is the 5 sense: something you can smell, see, hear, taste, touch.
3.Mindfulness: practicing mindfulness focuses on the present moment similar to grounding, but focusing on self awareness to help diminish sensations and promote relaxation. There are a few ways to do this and guidance can be helpful! Some examples include: EFT Tapping, Somatic Tracking, guided meditations. All offered in Vestibular Group Fit and interviews to learn more!
4.Movement/Exercise: Exercise and movement has many health benefits but has vestibular benefits as well. Exercise can help with stress, anxiety, depression, improved sleep, improved energy, reduce migraine attacks, and help build repetition and tolerance to daily movements. Progressing and scaling exercise has many benefits and translation to daily activities that are challenging. Talk to your doctor for clearance for exercise and consider consulting a provider to assist with progressing movement!
5.The Basics: Good and consistent sleep, proper hydration, healthy well balanced meals/snacks are relatively immediate and low cost changes to make in daily routines. This provides foundation for the body to have space for recovery and resources to help dedicate to recovery. Lots more on this in Vestibular Group Fit.
6.Professional Help: It takes many professionals that are experts in their own area to best assist and give tools for management. Finding the right profession, and then the right provider can be challenging, and one reason having a community for support and ask for recommendations can help find the right profession and provider faster. Someone like a headache specialist, neurologist with vestibular condition experience, or a vestibular practitioner can help!
In Conclusion
Living with anxiety-induced dizziness can be challenging, but it doesn’t have to define your life. By implementing these coping strategies and seeking support when needed, you can reclaim control over your well-being. Remember, it’s okay to ask for help, and you’re not alone in your journey toward managing anxiety in an effort to manage dizziness. Embrace these coping techniques, and empower yourself to thrive despite the challenges.
Incorporating these coping strategies into your daily routine can help alleviate anxiety and stress; ultimately helping with dizziness and empowering you to navigate life with greater confidence and resilience.
Want to learn more about mindset strategies to assist with managing anxiety and stress, as well as other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Sources
“Tips and Strategies to Manage Anxiety and Stress.” Anxiety and Depression Association of America, ADAA, adaa.org/tips. Accessed 22 Apr. 2024.