What is the Best Treatment for BPPV?
Benign Paroxysmal Positional Vertigo (BPPV) is a common cause of vertigo, characterized by brief episodes of dizziness triggered by changes in head position. This condition occurs when tiny calcium particles (otoconia) in the inner ear become dislodged and enter one of the semicircular canals, leading to a sensation of spinning.
BPPV Background and Anatomy
Otoconia are calcium carbonate crystals that reside in the utricle and saccule. The utricle and saccule help detect linear motion (up/down, forward/backward, side to side, tilting). The otoconia assist in this by responding to gravity which sends signals to the brain to interpret motion. Imagine a jar full of pebbles, tilting the jar will cause the pebbles to change distribution. The brain can take information like this and understand which direction the head is tilting, and direction of movement.
The semicircular canals are filled with a fluid called endolymph, and the job of the semicircular canals is to sense rotational movement. There are three canals positioned in different angles to detect different types of motion. As the fluid (endolymph) moves at various speeds in the different canals, tiny hair like cells called cilia move, and the brain is able to determine direction of movement and change in speed of movement. So what happens when a otoconia crystal winds up in the endolymph fluid of a semi circular canal? BPPV
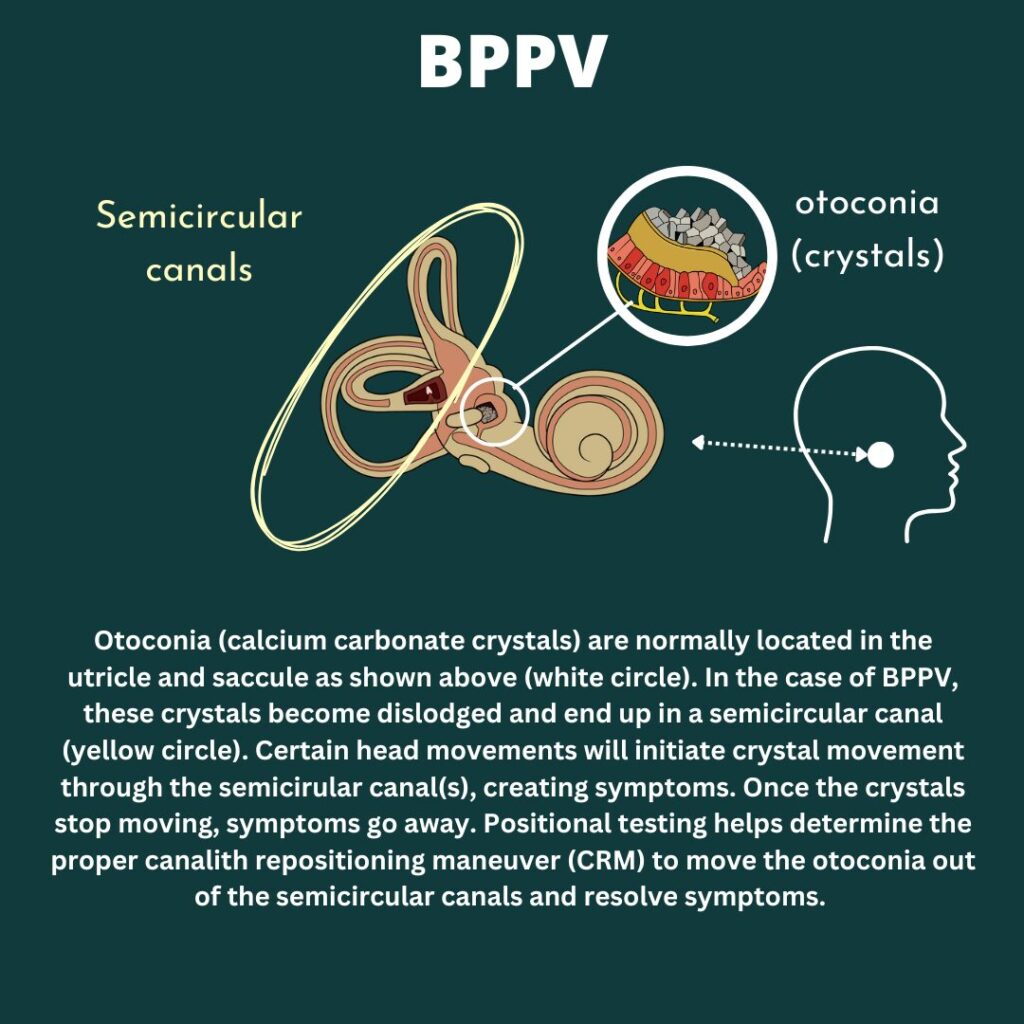
BPPV results in short, intense sensation of room spinning. This is brought on typically with certain head or body positions. As a provoking head position is brought on, the otoconia/crystals are encouraged to start moving due to gravity’s pull. As the otoconia move through the canal, this changes the rate the endolymph moves in the affected canal(s). This results in the brain getting mismatched signals from the vestibular systems and symptoms of dizziness, unsteadiness, room spinning, nausea, anxiety, sweats etc.
Vestibular information tells the brain movement information to help with balance and knowing where the body is in space. This information also helps the brain direct the eyes in the same direction and speed of the body for smooth gaze (vestibulo-occular reflex). With BPPV, the brain is getting multiple signals and is trying to have the eyes follow, resulting in nystagmus. Nystagmus is an involuntary, rhythmic eye movement. This can happen for other reasons, and can occur in different directions. This is helpful when testing, diagnosing and treating BPPV.
Assessing BPPV
Assessment for BPPV involves positional testing. This includes head and body movements while assessing for symptoms and any eye nystagmus. Each portion of the assessment is important in an accurate BPPV diagnosis and determining the correct maneuver to treat the involved canal(s). Positional testing assessing each canal. Determining which position recreates what someone has been feeling, and noting the direction of nystagmus helps determine which canal(s) and which side (left or right) is involved. This guides proper set up and treatment for BPPV.
Treatment for BPPV
Canalith repositioning maneuver (CRM) is commonly used to treat BPPV. It is important to properly assess the correct side and canal involved to choose and set up the correct CRM. The goal of CRM is to have otoconia travel through the semicircular canal and fully clear out of the canal to resolve symptoms. The Epley maneuver is a very common and successful treatment for posterior canal BPPV. If another canal is involved, other maneuvers is needed. A vestibular physical therapist can assess and determine next steps. Other providers that may address this can include ENTs or chiropractors but on an individual basis.
There are no medications that treat BPPV. There are some medications that can be helpful during treatment to better tolerate any dizziness or nausea. In rare instances, surgery can be performed to plug the posterior semicircular canal. This includes it’s own risk such as hearing loss and best to be discussed with a medical professional.
There are ways to treat BPPV at home. Assessment is still important to determine if symptoms are in fact BPPV and identifying the proper maneuver to set up. Some people have the same side and canal each time and will be taught at home CRM by their provider that they have seen for BPPV treatment. If recurrence is few and far between, or can involve different canals, the healing vertigo app is a great resource when at home, out of town, or needing guidance on positional testing and determining the proper home set up.
Guidelines for BPPV Treament
Typically, I recommend 2-3 maneuvers in a session and then give a day or two to see what’s improved. It’s normal to feel “off” or worse after a treatment session and then feel overall better once given some time to recover. Sometimes people feel immediately better after a session, other’s don’t, and they both be cleared of BPPV. Allowing 1-2 days post treatment can get a better idea how one is really feeling after allowing the body time to recover after treatments. Treatment does recreate dizziness in order to move the otolith through the canal, and why people can feel worse after, and why medications can help make treatments more tolerable. This is just a starting point and can be adjusted based on the person. Sometimes I’ve done one maneuver, other times five or more, it just all depends!
Some recommend avoiding certain movements, this is okay to a point, but avoiding movement forever or being afraid to move is not the end goal. Taking a day to avoid larger bending or laying flat is okay for comfort, but getting back into basic routine will ultimately give the feedback needed to determine if more treatment or assessment is needed.
Sometimes BPPV is cleared and certain movements can feel “off” as the body adjusts to vestibular systems with cleared BPPV. Some vestibular rehabilitation therapy and balance work can help after BPPV treatment and clearance to help any lingering or residual sensations.
Want to learn more about BPPV treatment and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://thevertigodoctor.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Dizziness triggers: threshold theory and 10 contributors to dizziness
Many are on the hunt for dizziness triggers. “What is the one or two things that make my dizziness worse”. “If I just figured out my trigger I can get rid of it and not be dizzy anymore”. The many variables in day to day life, both within and outside our own control, makes this a futile effort. This leads to feeling overwhelmed, hopeless, frustrated, and depleted. This article will discuss a different approach known as threshold or bucket theory as well as considerations of what may contribute to one’s threshold. We’ll also cover ways to track this and create a bigger threshold for long term growth and management.
What is threshold (bucket) theory? Why is this better than finding specific dizziness triggers?
Finding specific dizziness triggers or the root cause to dizziness sounds great in theory but much harder in practice. Each day is different, making this hard to track. There might be areas that might contribute to dizziness but is outside anyone’s control (weather, infection, allergies) so then what?
Threshold or Bucket Theory helps account for the variability of life, things within our control and outside our control, and why it’s rarely just one thing. Think of a bucket, and dizziness triggers fill up the bucket. Different things may fill up the bucket more or less on different days. On better days we might have a bigger bucket, on less ideal days the bucket is smaller. When the bucket starts to reach full capacity or even starts to overflow, symptoms are heightened or even a full on attack.
Looking at what may contribute to ones bucket can help strategize and know what days may be more challenging and more support is needed, see what is within our own control to be modified, finding grace for things outside ones control, and working on growing a bigger bucket.

Contributors to threshold (or possible dizziness triggers depending on the day)
The picture above illustrates threshold theory and common “dizziness triggers” or contributors to ones threshold. This better shows how it’s rarely one thing that sets off a dizziness flare or attack and more likely a combination of factors, including a lower threshold/smaller bucket. Listed below are common contributors, and we’ll go into a bit more detail in the next section.
- Stress
- Poor Sleep
- Poor Hydration
- Hormones
- Weather Changes
- Illness/Sickness
- Dizzy Anxious Cycle
- Environment
- Seasonal Allergies
- Muscle tightness/Lack of MovementLet’s dive deeper into each of these topics below!
- Stress: High levels of stress can exacerbate vestibular symptoms by triggering physiological responses like the fight or flight response. Stress can tie into the dizzy anxious cycle but can be it’s own separate contributor as well. Chronic stress can lower ones threshold can lead to other health impacts such as poor sleep, muscle tension, headaches, high blood pressure and more.
2. Poor Sleep: Inadequate or poor-quality sleep can disrupt the body’s natural rhythms and impair cognitive function and processes that help with memory and learning. Learning is an area that’s important when healing and recovering from vestibular conditions as part of positive neuroplasticity. Learning and brain function help with reweighing of the sensory systems (why Vestibular therapy works!) Sleep deprivation can lower ones threshold by making it harder for the brain to carryout tasks. With a vestibular condition, the brain is working harder to determine spatial orientation and movements, and trying to determine the correct response. When functions require more resources, sleep is important to optimize function.
3. Poor Hydration: Dehydration can disrupt the balance of fluids and electrolytes in the body, affecting blood pressure and circulation. This may be important in certain populations such as those with POTs (Postural Orthostatic Tachycardia Syndrome). Being properly hydrated is again important to best support the body for healing and recovery.
4. Hormones: Fluctuations in hormone levels, such as those experienced during menstruation, pregnancy, or menopause, can influence vestibular function and trigger dizziness. There are some blog posts that go into more detail on the website. But there’s some amazing in depth information and discussions for Vestibular Group Fit Members.
5.Weather changes: Variations in barometric pressure, temperature, and humidity can contribute to ones threshold. Think of weather as a possible stressor to the body. Sudden changes in weather conditions may lower the threshold for dizziness and vertigo, especially for individuals with sensitivity to atmospheric pressure changes. The weatherx app and ear plugs can better assist tracking possible connections to barometric pressure shifts, and weather x ear plugs to assist in minimizing the impact of the weather.
6. Illness/Sickness: Viral infections, bacterial illnesses, and other health conditions can add stress to the body. As the body is fighting off an infection, energy and resources are being diverted to fight off an illness. Illness-related symptoms may lower the threshold for experiencing vestibular symptoms, particularly during periods of acute illness or recovery.
7. Dizzy-Anxious cycle: The relationship between dizziness and anxiety can create a vicious cycle where dizziness triggers anxiety, and anxiety exacerbates dizziness symptoms. This cycle can quickly fill ones threshold. This cycle can be broken, and why mindfulness and mindset work is so so important. Consider a professional to assist with tools and coping strategies. A whole section on medications, breathwork, and tools are in Vestibular Group Fit for members to explore.
8. Environment: Environmental factors such as noise, lighting, and visual stimuli can worsen dizziness. Certain environments, such as crowded or visually stimulating spaces, may lower ones threshold as well if visual vertigo or motion sensitivity is part of ones vestibular condition (hint: it is for many).
9. Seasonal allergies: Allergic reactions to pollen, dust, or other environmental allergens can exacerbate inflammation and congestion in the sinuses and even feel like plugged ears. Seasonal allergies may lower the threshold for experiencing dizziness and vertigo, especially during peak allergy seasons, everyone responds to allergies different, but springtime can be tough for vestibular warriors between weather shifts and pollen counts.
10. Muscle tightness/Lack of movement: Muscle tightness, especially in the might back, upper trap and neck region can impact migraine conditions and dizziness. Muscle tightness and resulting pain or a state of discomfort can make other symptoms worse as well. The body likes to move, and having tight, stiff, painful muscles or a fear of movement from dizziness and unsteadiness can become a vicious cycle.
How to track dizziness triggers or your threshold contributors
Using apps like Migraine Buddy or keeping a symptom journal can be valuable tools for tracking possible dizziness triggers in individuals with vestibular disorders. However, it’s important to approach symptom tracking mindfully to avoid hyperfocus, which can exacerbate symptoms and diminish quality of life. Rather than constantly monitoring, it’s recommended to track symptoms after noticing an increase or flare in dizziness.
Record information from the past 1-2 days, things like:
- hormonal fluctuations.
- stress levels
- weather
- allergies
- meals (skipped meals, different meal times, missed a bedtime snack, less nutrient dense meal etc)
- sleep
If experiencing increased symptoms or a flare, consider tracking symptoms leading up to the event, any medications taken, and strategies employed for relief. This can help identify patterns or prodromal signs preceding an attack and evaluate the effectiveness of medications or interventions. Remember, the goal is not to obsessively monitor every moment, but to gather insightful data that can inform targeted interventions and improve symptom management over time.
How to get a bigger threshold
Growing a larger threshold over time to better manage vestibular disorder symptoms involves a holistic approach that encompasses various aspects of health and well-being. Luckily, some of these are little to no cost, no doctors prescription needed. Building a bigger bucket does require consistent routine changes. Start small start slow. Build up a new routine one thing at a time, then add another. Check out a podcast on this here.
Just a reminder as well, certain factors like allergies, weather fluctuations, or illness may be beyond our control. Focusing on strategies within our control can help grow a larger threshold over time, allowing us to better absorb dizziness triggers we cannot control. There are some tools to try such as Weather X ear plugs before barometric pressure shift, allergy medication or natural nasal spray, measures to reduce risk of illness during cold and flu season. These may be good and useful tools to implement based on the situation.
Ways to grow a bigger bucket:
- Consistent, high-quality sleep is fundamental, as it supports overall health and resilience to stress.
- Regular movement, tailored to individual capabilities, promotes physical strength and balance, while staying adequately hydrated ensures optimal functioning of bodily systems.
- Engaging in mindset work and stress management techniques can help cultivate resilience and reduce the impact of stressors on symptoms.
- Environmental changes/workplace accomodations such as blue light glasses like avulux, blue light filters for computer use like iris tech, light covers for overhead fluorescent lighting, loop ear plugs etc.
- Seeking assistance from healthcare providers and building a supportive provider team can offer valuable guidance and resources for symptom management.

Living with a vestibular disorder requires patience, resilience, and a proactive approach to managing triggers and symptoms. By incorporating lifestyle modifications, stress management techniques, and awareness of your personal threshold, you can take control of your condition and improve your overall well-being. Remember, you’re not alone in this journey, and seeking support from healthcare professionals and fellow individuals living with vestibular disorders can provide valuable guidance and encouragement. Together, we can navigate the challenges of dizziness and find moments of stability and balance in our lives.
Disclaimer
Want to learn more about threshold contributors, tools to manage contributors, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
7 Ways to find support for vestibular conditions
Having support for vestibular conditions in various aspects of life are essential for navigating this challenging journey. Vestibular conditions truly take a village of friends, family, providers, and professionals to help along the path to confident management. In this blog post, we’ll explore various avenues for seeking support and connecting with others who understand what you’re going through.
7 areas to find support for vestibular conditions
- Support Groups
- Counseling
- Return to Work Accommodations
- Medical Intervention
- Holistic Intervention
- Friends and Family
- Success Stories
1. Support for vestibular conditions: Support groups
In today’s digital age, online communities have become invaluable sources of support and solidarity. Platforms like Facebook groups, Reddit communities, and online forums host discussions where individuals share experiences, coping strategies, and encouragement. Joining these groups can provide a sense of belonging and reassurance that you’re not alone in your journey. There are some great vestibular warriors and providers that help host local and online support groups. Here’s some resources on finding one to join.
2. Support for vestibular conditions:
Counseling
Living with a vestibular condition can take a toll on your mental health, leading to feelings of anxiety, depression, or isolation. Seeking counseling or therapy can be immensely beneficial in navigating these emotional challenges. A professional can help provide a safe space to vent and work through challenging emotions and grieving that is so normal to arise. It can be hard to find a professional that knows both counseling and vestibular conditions. One provider that does is Dr. Emily Kostelnik (The Vestibular Psychologist) Who is a licensed clinical health psychologist and fellow vestibular warrior. Her and her team of mindset coaches are great to work with. Other options for support for vestibular conditions include a therapist that has background in chronic pain. Chronic pain can have similar overlap to chronic dizziness. Finding a provider can be done through different databases. Feel free to check out here & here. It can take some time to find a counselor that really clicks; it’s okay to switch therapists!
3. Support for vestibular conditions: Return to work accommodations
Vestibular conditions make most, if not all, jobs challenging to complete. This does not mean returning to the same job can never happen. People have returned to work. This can look like a gradual return to work program and/or requesting reasonable accommodations to support job tasks. Going part time and building up hours, blocking off certain parts of the day to space out challenging tasks, requesting an office location that is quiet, remote work etc. More on this in a blog post here. The Job Accommodation Network is a great resource as well to learn what accommodations are common with dizziness, and prompts to help determine what may be requested based on specific job tasks. Return to work can include a combination of other interventions as well as modifications to best give support for vestibular conditions.
4. Support for Vestibular Conditions: Medical intervention
Navigating the medical side of vestibular conditions can be murky. Understanding how the vestibular system works (video here). Can turn fear into empowerment. Understanding which providers can be helpful or finding ones to team up and help create a management plan can help give the body the support needed to recover. Navigating specialists, tests, and various treatment routes can be hard to do alone. Having resources and community from others who have experienced this can help.
5. Support for Vestibular Conditions: Holistic intervention
Holistic work has its own seat at the table. Meditation, mindfulness, tai chi, yoga, herbs, supplements, guided visualization are different ways a holistic approach can be incorporated. Finding calm and safety is important for taming the dizzy anxious cycle and rewiring movements to mean safety. Finding self compassion and acceptance is huge here as well.
6. Support for Vestibular Conditions: Friends and family
Finally, don’t underestimate the power of building a personal support network comprised of friends, family, and loved ones. Communicate openly with those close to you about your condition, how it impacts your life, and what support you need. Their understanding and empathy can provide a strong foundation of support as you navigate the ups and downs of living with a vestibular disorder. This can be challenging and something talked about in detail within small group coaching and Vestibular Group Fit. Check out this episode that discusses dating, or this blog.
7. Support for vestibular conditions: Success stories
Knowing you aren’t alone is a huge weight off ones shoulders. But what about next steps? Or hope for the future? Hearing others journeys and successes is an uplifting reminder that you aren’t alone and it does get better. Here are some written options, and more with audio at Grounded: The vestibular podcast
Vestibular Group Fit
All this and more can be found in Vestibular Group Fit. This low cost monthly subscription has education, community, support and guidance to answer your questions and find your path to healing and management. Learn about the ‘why’ here.

Disclaimer
Want to learn more about strategies, information, tools and support for vestibular conditions? Get vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
5 Habits to Help vertigo and dizziness: A guide towards relief
Vertigo and dizziness can be disorienting, isolating, frustrating, and challenging to navigate. Learn how to help vertigo and dizziness in daily habits. In this article you’ll find information on daily habits that can assist in management of dizziness, and strategies that are discussed in detail with subscription to Vestibular Group Fit. There will be some discussion on other routes to compliment these habits but this list is not exhaustive. This list is designed to show common habits that have helped others, and can be relatively low cost or free to instill, with no prescription from a doctor needed.
5 Habits to help vertigo and dizziness
- Hydration. Many many people are not properly hydrated. Ensuring proper hydration is a daily habit that can better support the body and vestibular system. Many find adding electrolytes to help their hydration has assisted with brain fog, dizziness, energy etc. Talk to your doctor before adding electrolytes to your diet
- Stress and Mindset Management. One of the largest contributors to migraine attacks is stress (the other poor sleep we’ll talk about later). Stress can act like gasoline on the smallest of embers to really light up a fire. Being able to have coping mechanisms to address stress, as well as tools to modify or adjust stressors that are within control is important for overall quality of life as well as vestibular, vertigo and dizziness management.
- Nutrition. Sometimes diet changes such as limiting alcohol or caffeine intake can be helpful. This can also help anxiety and sleep quality. Adding healthy fruits and vegetables to have a well balanced diet to include protein, carbs and fats is helpful for stabilizing blood sugar and can help with overall health but also dizziness. Protein and well balanced meals and snacks have helped others reduce or eliminate later afternoon crashes, middle of the night or morning attacks. Making dietary changes should be discussed with your doctor prior to making changes, and consider a professional nutritionist or dietician for further assist and guidance.
- Movement. The body craves movement. The vestibular system helps measure movements and the brain takes those signals to make any adjustments to stay safe. Movement helps with strengthening the connection between vestibular system and the brain. Movement helps with stress, anxiety, improved sleep, improved health, hormones and so much more. This is a pillar of Vestibular Group Fit and is important to start small and gradually progress. Slow and steady. Gentle movement such as a short walk, gentle yoga or tai chi. Beginner workouts or dance classes are all great options (and also included with modifications and considerations for vestibular conditions in Vestibular Group Fit) Discussing with your doctor before performing a new exercise program is encouraged.
- Sleep. Quality, consistent sleep helps healing and giving the brain and body the rest it needs to learn, rewire and heal. Consistent sleep wake times, even on the weekends, setting up a bedtime routine, and getting quality sleep is again, important for general health but also long term management of vertigo and dizziness.
- Switch to natural options when possible. Switching to natural cleaners, soaps and detergents can take possible irritants out of the home. Brands like Branch Basics help make this easy!

Other considerations to help vertigo and dizziness
The habits mentioned above can be great to help vertigo and dizziness. Some notice considerable change when changing habits, others notice the benefits after staying consistent for 3-4 months. Others notice this has helped support other treatments to feel their best.
Other treatments, providers, or interventions may be needed for the right resources, or to help get the body to a place where daily habits can act as a considerable part of management.
This may look like medications to help break the dizzy anxious cycle, vestibular rehab therapy to scale movements back to daily routines, vision therapy to address visual symptoms, neuro modulation devices, Botox injections, and having medications to prevent or stop attacks from starting.
This can look different to everyone as everyone’s situation and background is unique to them which is why this list is not exhaustive but mean to highlight common habits that help. More resources, information and recommendations exist in Vestibular Group Fit by both expert vestibular practitioners and other vestibular warriors with their own knowledge, experience, and support.
Living with vertigo and dizziness can be challenging, but it’s essential to remember that relief is possible. By incorporating these practical tips into your daily routine, you can better manage your symptoms and regain control over your life. Remember to consult with a healthcare professional if your symptoms persist or worsen, as they can provide personalized guidance and support on your journey toward wellness.
Disclaimer
Want to learn more about daily habits to help vertigo and dizziness as well as other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Managing Anxiety and Stress to Help Dizziness
Your head spins, the room seems to sway, and suddenly, your heart races. If you’ve ever felt this, you’re not alone. Anxiety and stress can make dizziness worse. However, understanding the connection between anxiety and dizziness and learning coping strategies can greatly alleviate its impact on your daily life.
Overview: Dizzy Anxious Cycle
The dizzy anxious cycle is so important in learning about and addressing for best results and management. This can be a ‘chicken or the egg’ scenario, but dizziness can bring on anxiety, anxiety can make dizziness worse, worsening dizziness makes anxiety worsen and on and on this cycle can spiral. Working on breaking this cycle can be a game changer for dizziness. This can be done a variety of ways and different professionals to assist. More on the dizzy anxious cycle in a blog here, or podcast here.

Overview: Dizziness and Stress
Stress has a tendency to act like gasoline on a fire. Now there is such a thing as good stress. Lifting weights or running faster/longer distances are technically stress to the body, but helps promote adaptations and progress in a way that benefits the body long term when done correctly. Good or bad, stress can take a toll on the body, especially when the body is under more stress than it can tolerate.
Dizziness and worsening symptoms adds stress to the body, making it hard to tolerate other stressors. Some stress we can be in control of, other times source of stressors are outside our control. Learning how to manage stress, especially stress outside our control, is important part of dizziness progress and management. Learning how to react to stress creates a ripple effect through emotions, attitude/mindset, and actions.
Overview: Depression and Grieving with Dizziness
While taking time to talk about anxiety and stress, depression or grief may be mixed in with these other emotions. Dizziness can be accompanied with feelings of depression, loss, and mourning of “life before dizziness”. These feelings are valid and real and should be processed in order to find coping strategies and work towards growth. This may need to be done with professional guidance. Check out this website to help find a mental health therapist to work with.
Managing Anxiety and Stress
Thankfully, there are effective coping strategies to manage anxiety and stress. Drawing insights from the Anxiety and Depression Association of America (ADAA), as well as anecdotal advice from other vestibular warriors and vestibular therapists, here are some practical tips to regain control:
- Breathwork
- Grounding
- Mindfulness
- Movement/Exercise
- The Basics
- Professional Help (linked here is another source to help find professional help)
We’ll get into the specifics below with examples of each.
1.Breathwork: There are a variety of breathing techniques that can help with relaxation. The goal of these techniques is to tap into the “rest and digest” part of our nervous system and help turn off the fight or flight system. Finding what works best for you is the goal. Deep, slow breaths is the goal.
Some examples are: yoga breathing, box breathing, triangle breathing, alternating nostril breathing, physiologic sigh etc.
2. Grounding Grounding is aimed to help anchor you to the present moment. This is helpful when not feeling connected to ones body and feeling disassociated.
Try the 5-4-3-2-1 method: identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste.
Another example is the 5 sense: something you can smell, see, hear, taste, touch.
3.Mindfulness: practicing mindfulness focuses on the present moment similar to grounding, but focusing on self awareness to help diminish sensations and promote relaxation. There are a few ways to do this and guidance can be helpful! Some examples include: EFT Tapping, Somatic Tracking, guided meditations. All offered in Vestibular Group Fit and interviews to learn more!
4.Movement/Exercise: Exercise and movement has many health benefits but has vestibular benefits as well. Exercise can help with stress, anxiety, depression, improved sleep, improved energy, reduce migraine attacks, and help build repetition and tolerance to daily movements. Progressing and scaling exercise has many benefits and translation to daily activities that are challenging. Talk to your doctor for clearance for exercise and consider consulting a provider to assist with progressing movement!
5.The Basics: Good and consistent sleep, proper hydration, healthy well balanced meals/snacks are relatively immediate and low cost changes to make in daily routines. This provides foundation for the body to have space for recovery and resources to help dedicate to recovery. Lots more on this in Vestibular Group Fit.
6.Professional Help: It takes many professionals that are experts in their own area to best assist and give tools for management. Finding the right profession, and then the right provider can be challenging, and one reason having a community for support and ask for recommendations can help find the right profession and provider faster. Someone like a headache specialist, neurologist with vestibular condition experience, or a vestibular practitioner can help!
In Conclusion
Living with anxiety-induced dizziness can be challenging, but it doesn’t have to define your life. By implementing these coping strategies and seeking support when needed, you can reclaim control over your well-being. Remember, it’s okay to ask for help, and you’re not alone in your journey toward managing anxiety in an effort to manage dizziness. Embrace these coping techniques, and empower yourself to thrive despite the challenges.
Incorporating these coping strategies into your daily routine can help alleviate anxiety and stress; ultimately helping with dizziness and empowering you to navigate life with greater confidence and resilience.
Want to learn more about mindset strategies to assist with managing anxiety and stress, as well as other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Sources
“Tips and Strategies to Manage Anxiety and Stress.” Anxiety and Depression Association of America, ADAA, adaa.org/tips. Accessed 22 Apr. 2024.
Coping with dizziness and vertigo
Dizziness can be a disconcerting and often debilitating sensation, especially when it strikes unexpectedly. Coping with dizziness and vertigo can be done through a variety of ways including lifestyle changes, medications, medical and holistic interventions.
While medical interventions and treatments play a crucial role in managing dizziness, incorporating lifestyle modifications can also be incredibly beneficial. By making simple yet effective changes to our daily routines and habits, we can better cope with and reduce the frequency of dizzy spells.
Understanding dizziness
Before discussing methods for coping with dizziness and vertigo, we’ll do a brief overview of dizziness and vestibular conditions. If you’d like to learn more, this blog post goes into more detail. Vestibular conditions can result in symptoms of dizziness and vertigo as well as: light headedness, bouncing vision, rocking, swaying, brain fog. Secondary symptoms can also include anxiety, fear, depression, fear to leave the home. More on symptoms, anatomy and triggers for symptoms here.
Vestibular conditions result in inaccurate, incorrect, or delayed relaying of information to the brain. The brain takes in information from the vestibular system, visual system and proprioceptive system to determine where the body is in space, and any corrections needed in order to stay safe. If there is a mismatch in signaling, the error signal produces unwanted symptoms. Since we are dealing with spatial orientation and movement, many find quick movements, repetitive movements, or general balance to be challenging and aggravating.
It’s normal to having additional testing to rule out other causes such as medication toxicity, stroke, MS, cardiac involvement, POTS etc. There are tests to help determine vestibular involvement through ENT/audiology or with a physical therapist. More on this here and here.
Identifying the underlying cause of your dizziness is crucial for effective management.
Coping with dizziness and vertigo
Back to the Basics: these areas are probably something we’ve all been told to help support healthy habits and support the body. Many are low cost or free and tend to be overlooked at the impact they can have.
-
- Hydration. Up to 75% of Americans are chronically dehydrated(1). Limiting caffeine and alcohol, and talking to your doctor about electrolytes to assist with improving hydration can be helpful for dizziness.
- Diet. Aim for a balanced diet with fresh fruits, vegetables, grains, fats and protein. Reducing processed foods and inflammatory foods can help with gut health which can be beneficial overall and help with dizziness.
- Sleep. Consistent, good quality sleep is so important. A bad night sleep can make the healthiest person feel subpar. Getting enough sleep and regular sleep becomes even more important with vestibular conditions.
- Stress/Mindset. Working on mindfulness to help with stress and outlook has been a game changer for many with dizziness in getting back to their favorite activities or getting over a plateau. There’s a lot of resources and different ways to practice mindset, many are compiled for you and regularly updated in Vestibular Group Fit.
- Movement. There are many benefits to exercise for health, stress management, improved sleep, but can also help with dizziness. Exercise can help reduce migraine attacks and can also help work on functional strength and movements to return to activities. Starting gradual and slow is important, and is recommended to talk to your doctor and physical therapist for further guidance to get started.
Research has shown that the top 3 stressors for those with migraine attacks are sleep, stress and fatigue (2). When thinking of vestibular migraine or vestibular conditions in general, these are huge in long term management for not just dizziness, but overall well being.
Additional considerations for coping with dizziness and vertigo
- Modifications. The goal is to return to daily activities, work and hobbies to ones fullest potential. In the meantime, making modifications is helpful not only in progressing towards goals, but participating in activities with reduced symptoms. This might include breaking down tasks throughout the day, prioritizing the main tasks, taking breaks. Other options include blue light glasses such as avulux to help with screens and overhead lights. If traveling a lot or experiencing altitude changes using earplanes, or tracking weather changes with weather X app.
- Supplements. Depending on the vestibular condition, certain supplements have been backed by research to help improve symptoms.
- Support. It takes a village. Having close friends be able to help during symptom flares. A medical team to assist with treatment, tests, and ongoing management. Mental health therapists to help with coping strategies for stress or anxiety. Finding others that understand your challenges due to having vestibular conditions themselves. Having a trusted circle is so important to celebrate the wins, and support during the set backs.
- Medical intervention. This may include medications to help prevent or abort an attack from starting. This may also include vestibular rehab to work on return to movements and daily activities. Headache specialists are helpful in mangement and diagnosing of vestibular migraine. Check out this provider look up tool here. If there isn’t one close by or you have a provider you trust and is open to a collaborative team approach, consider neurahealth for telehealth appointments with headache specialists that are well versed in vestibular conditions. Click here to learn more and use VERTIGODOCTOR15 for a discount!
Remember, small changes can yield significant results, empowering you to live life to the fullest despite the challenges of dizziness.
Disclaimer
Want to learn more about management strategies and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources
- Taylor K, Jones EB. Adult Dehydration. 2022 Oct 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32310416.
- Park JW, Chu MK, Kim JM, Park SG, Cho SJ. Analysis of Trigger Factors in Episodic Migraineurs Using a Smartphone Headache Diary Applications. PLoS One. 2016 Feb 22;11(2):e0149577. doi: 10.1371/journal.pone.0149577. PMID: 26901341; PMCID: PMC4764678.
Diagnostic testing for vestibular disorders-explained
Entering the realm of diagnostic testing for vestibular disorders can be overwhelming, to say the least. But fear not; this guide aims to shed some light on the process, helping you navigate through the labyrinth of medical terminology and procedures.
When first going to a doctor for dizziness, it’s normal for tests to be ordered to gather more information as to what might be going on. Below are common diagnostic testing for vestibular disorders to assist providers in gathering more information on the function of each vestibular organ. These are commonly performed by an audiologist. Other tests performed by a physical therapist are in detail here.
Taking into account each individuals story is so important. Your provider will listen to your experience, consider other medical history factors to assist in further referrals. Typically an MRI or CT scan will be ordered to rule out other causes. In most cases, this type of imaging will come out normal in those with vestibular conditions. MRI and CT scans are not great at finding vestibular related conditions. MRI and CT are good at ruling out other causes (stroke, tumor, MS etc).
CT scan is useful with identifying Superior canal dehiscence or thinning of the temporal bone. Symptoms such as “hearing your eyeballs move” or dizziness with sneezing or coughing are common symptoms that prompt this type of imaging. In most other cases however, MRI and CT scan are just the beginning of tests. Below includes testing to determine the status and function of the vestibular system.
Quick vestibular system background
Let’s quick talk about what it is that we’re testing–the vestibular system. The vestibular system, nestled within the inner ear, plays a pivotal role in maintaining balance and spatial orientation. When this delicate system becomes disrupted, whether due to injury, infection, or other underlying conditions, it can wreak havoc on your equilibrium, leading to a myriad of symptoms such as dizziness, vertigo, nausea, difficulty concentrating, unsteadiness, neck pain and more. Diagnostic testing for vestibular disorders looks at directly testing the nerve the shares information between the vestibular system and brain to determine possible diagnoses.
Diagnostic testing for vestibular disorders
Listed below are common tests used to gather more information. This information can assist with other physical assessments and personal report to help with diagnosis and moving forward with a treatment plan.
- Electronystagmography (ENG): This test tracks your eye movements in response to various stimuli, helping to identify abnormalities in the vestibular system.
- Videonystagmography (VNG): Similar to ENG but utilizing infrared video technology for more precise measurements of eye movements. This includes tracking objects, looking between targets and other eye movements. Positional testing to assess any dizziness when in different head and body positions are performed with eye movement recorded and measured. This can help identifying any signs that don’t indicate a vestibular/peripheral cause, and other conditions such as BPPV.
- Caloric Testing: By stimulating each ear with warm and cool air or water, this test assesses the superior branch of the vestibular nerve. Movement sensations are a very normal sensation to have here. It is not an attack. The temperature differences is stimulating only one side of the vestibular system on purpose. This produces involuntary eye movements (nystagmus). By comparing one side to the other. This test looks for symmetry of each vestibular signal and can help identify asymmetries.
- Rotary Chair Testing: You’ll be comfortably seated in a rotating chair while your eye movements are monitored, providing valuable information about your vestibular function.
- Vestibular Evoked Myogenic Potentials (VEMP): This test evaluates the inferior branch of the vestibular nerve which helps with the otolith and saccule function. This involves electrodes on the head/neck with some head movements and sounds. This can help in diagnosing: vestibular neuritis, Meniere’s disease, superior semicircular canal dehiscence.
- ECOG (electrocochleography Exam): This looks for increased fluid pressure in the inner ear. This can be indicative of Meniere’s disease. This test is not used in isolation to diagnose Meniere’s disease as this test isn’t as accurate if being done in between attacks. This involves some electrodes and a few sounds played. A relatively quick and easy test!
- Audiogram: A basic hearing test can help determine any hearing loss and what type. Meniere’s disease can cause low frequency hearing loss on the affected side. Labyrinthitis will also cause hearing loss.
- Auditory Brainstem Response (ABR): Similar set up to an ECOG this test helps measure for any hearing loss. Typically this is done in those that are unable to perform an audiogram.
Other considerations
Other considerations include vision exams to determine a need for vision therapy, or blood work to determine thyroid function, any deficiencies, or inflammatory markers in bloodwork that may be contributing to symptoms. These areas might not be explored initially, but are good to keep in mind as more information is gathered.
There are also additional tests that can help indicate vestibular involvement performed by a physical therapist. More on that in the blog post here. For more info on what to expect during testing, check out this post here
To learn more
Want to learn more about testing, diagnoses, and listen to an interview with a vestibular audiologist? Learn about other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Tests for a vestibular diagnosis
Imagine seeking answers for persistent dizziness, only to find yourself shuttled between neurologists for MRI or CT scans, ENT specialists for auditory and balance testing, and even cardiology to rule out heart-related issues—all to no avail. You’re left bewildered, feeling anything but normal, despite test results consistently coming back within normal ranges. This frustrating journey is all too familiar for many individuals grappling with vestibular disorders. However, the key lies not in the conventional diagnostic avenues, but rather in understanding the intricacies of vestibular diagnosis.
Vestibular system background
The vestibular system, alongside proprioception and vision, plays a crucial role in maintaining balance and spatial orientation. Situated within the inner ear, the vestibular apparatus comprises semicircular canals and otolith organs, which detect rotational and linear movements, respectively. When this system malfunctions, individuals often experience a myriad of symptoms, including vertigo, dizziness, imbalance, nausea, and visual disturbances. These symptoms can significantly impair daily life, affecting mobility, productivity, and overall well-being.

Vestibular information is used in two ways. One is for balance, and the other is to keep our eyes focused and steady on a target, even while moving. For this to happen, information needs to be sent from the vestibular system to the brain. Certain systems and reflexes are designed to take this information and perform the necessary movements of the head, neck, trunk and eyes to do this seamlessly.
There is also an additional pathway that connects the vestibular system to the autonomic nervous system called the vestibulo-auntomic pathway. Knowing the different pathways the vestibular system is used in can help explain a lot about symptoms. Unsteadiness, bouncing vision, anxiousness etc. This also helps explain tests performed to help determine a vestibular diagnosis.
Testing to determine vestibular involvement
To unravel the mysteries of vestibular disorders, a range of specialized tests and examinations are utilized. The tests below are something that can be expected during a clinical examination at a physiotherapist or physical therapists office. If interested in learning more about specific diagnoses, check out the list of more detailed posts here.
Nystagmus, characterized by involuntary eye movements, can provide valuable insights into vestibular function. The vestibular system helps in keeping vision stable, so involuntary eyes movements that act a certain way can give insight into what signals are being sent by the vestibular system and vestibular nerves.
Positional testing, particularly for benign paroxysmal positional vertigo (BPPV), involves maneuvering the head to provoke characteristic symptoms and identify the affected canal. Involuntary eye movement (nystagmus) is helpful in combination with positional testing to determine the involved side (left or right) and canal to perform the proper corrective maneuvers.
Dynamic Visual Acuity (DVA) testing assesses the ability to maintain clear vision during head movements, offering further clues to vestibular dysfunction. If there is inaccurate signaling or information, this test will yield abnormal results. Retesting can help determine progress being made.
Standing balance assessments, such as Computerized Dynamic Posturography (CDP) or modified Clinical Test of Sensory Integration of Balance (mCSTIB), evaluate postural stability under various conditions while manipulating the different sensory inputs used for balance. This gives insight into what conditions are challenging, and what sensory systems are involved.
Functional balance assessments like the Functional Gait Assessment (FGA) gauge the individual’s ability to perform everyday tasks requiring dynamic balance control. This ties the functional movement aspect that is so impactful with vestibular conditions. To include movements such as turns, stepping over objects, narrow walking, walking eyes closed, or walking with head turns helps determine troublesome movements for each individual. These types of test can also help build a rehab program and act as a retest to track progress.
Testing from other providers
Videonystagmography (VNG) and Vestibular Evoked Myogenic Potentials (VEMP), we delve deep into the function of the vestibular nerve branches, shedding light on the superior and inferior pathways. By assessing the integrity of these neural pathways, we gain invaluable insights into vestibular function. However, it’s essential to acknowledge the limitations—while VNG and VEMP offer vital information, they can’t capture every nuance of vestibular nerve activity. Consequently, normal test results don’t always rule out vestibular involvement, especially in conditions like vestibular migraine. This type of testing does include a hearing test, which can help determine conditions such as Meniere’s Disease. More on this type of testing here and here.
MRI: this can rule out central causes of dizziness such as MS, stroke, Parkinsons, cerebellar disorders, acoustic neuroma. This cannot diagnose a concussion or vestibular migraine, which can be a vestibular condition resulting in dizziness, but a normal test result. This type of test is important to rule out other possible causes, but can feel discouraging as a normal test result when you’re not feeling normal.
Cardiology workup, tilt table testing. This is an area that can result in dizziness with conditions such as atrial fibrillation. Screening for other areas such as orthostatic hypotension, or Postural Orthostatic Tachycardia Syndrome (POTS) should be considered with a cardiologist (sometimes this is neurology as well) to diagnose and assist with management.
In conclusion
Navigating the labyrinth of vestibular diagnosis demands a holistic approach, recognizing the unique challenges posed by vestibular disorders. While conventional testing may yield normal results, it is imperative to delve deeper into the vestibular system to uncover underlying dysfunction. By harnessing specialized tests and examinations tailored to assess vestibular function, individuals can finally find clarity amidst the dizzying array of symptoms. So, if you find yourself trapped in the cycle of unexplained dizziness, remember—it’s not just about normal test results; it’s about deciphering the vestibular puzzle to reclaim your equilibrium and quality of life.
Want to learn more about testing, diagnoses, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Renga V. Clinical Evaluation of Patients with Vestibular Dysfunction. Neurol Res Int. 2019 Feb 3;2019:3931548. doi: 10.1155/2019/3931548. PMID: 30863640; PMCID: PMC6377969.
How to treat long Covid dizziness in 4 steps
Research on COVID 19 has shown a variety of symptoms, with one study showing 19% of people report dizziness or vertigo as a symptom. This blog post discusses long covid dizziness and 4 steps to get your dizziness addressed. (1) Learn the latest research on long covid dizziness and steps to take to address covid related dizziness including common providers and treatments.
Research last updated August 2023 for this article. Ongoing research is occurring in this area so information discussed may be out of date depending on the time you read this article.
What is considered long Covid
The acute phase of covid is when symptoms first appear, and testing shows a positive result until your body has cleared the active virus. The acute phase by the CDC has recommendations ranging 5-10 days during this acute phase based on different scenarios you can find here.
Long covid is defined as symptoms that are present 4 weeks after the acute phase is over (2). About 10% of people with covid get long covid. There appears to be a link with increasing likelihood of long covid with each reinfection.
Dizziness and Covid
During infeciton, our body releases cytokines as part of the normal immune response. A cytokine storm is when the body release too many cytokines into the blood too quickly. This can be a result of infection, autoimmune condition or other disease. This can occur during covid 19 infection and is believed to be a contributor to long covid symptoms.
Meniere’s disease, vascular vertigo and BPPV have also been linked to elevated cytokines.
Covid related dizziness can appear in a variety of ways. Typical testing used by audiology for assessing for vestibular disorders shows abnormal findings in those with dizziness after covid (3). A variety of findings came from this study on testing, talking to your doctor about comprehensive testing with audiology or ENT could be a helpful step in determining best course of action.
How Covid or long Covid dizziness occurs
During infection, there are a few ways that the body can be involved that result in dizziness. Some are:
- It can trigger VM
- It can cut off blood flow to inner ear, presenting like a vestibular neuritis
- Trigger BPPV
- Disrupt neural pathways involved in balance
- Attack Schwann cells on vestibular nerve
- Attack hair cells in vestibular system
Long Covid dizziness and migraine
Other considerations with covid related dizziness is how this impacts others based on a variety of factors. For example, those with a prior history of migraine report intensified symptoms of their migraine attacks. If no previous history of migraine, the onset of headache or migraine disorder may become known. This is thought of a genetic link to a person with a higher susceptibility to migraine or dormant and infection activated the headache or migraine disorder.
Treatment: Treat like a migraine disorder. Get a headache specialist and/or neurologist involved. Work on breaking the cycle of migraine attacks and then focus on prevention and management.
Long Covid dizziness: Hypofunction
If your presentation after covid is like a neuritis or hypofunction, the same treatment principles apply. It appears that compensation for this can take longer than a traditional hypofunction/neuritis. Keep this in mind as you’re working on VRT, exercise, mindset etc. Progress can be made and good recovery, but it may take longer and that’s normal.
Treatment: Vestibular Rehab Therapy. ENT or PT are common providers to identify and manage this condition
Long COVID dizziness and POTs
POTs stands for Postural Orthostatic Tachycardia Syndrome. POTS symptoms can vary widely with more information from Cleveland clinic here.
79% of those with long covid meet criteria for Treatment regime generally consists of: graded exercise (recumbent/supine) , fluids and electrolytes, compression garments, smalls meals throughout the day, certain medications. Cardiology is an important provider role to have on your team for identifying and managing POTS.
Other treatment considerations for long Covid dizziness
- Determine what covid caused for you. (hypofunction, migraine, PPPD, BPPV etc.)
- Treat condition if there is one
- Manage the dizziness (Remember Vestibular Group Fit principles here: Movement, Mindset, Education, Medical support)
- Get moving! Not sure where to start? Consider being a vestibular group fit member for guidance, support and access for scaling movement content.
This is treatable and manageable. Getting the right providers to help manage and monitor your care with you is important!
Common medical providers for dizziness
Typical providers that are involved in this type of care are:
- post covid care centers
- internal medicine physician
- neurology
- ENT
- Cardiology (POTS)
Disclaimer
Want to learn more about long covid dizziness and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Sources
- 1. Caronna E, Ballve A, Llaurado, et al. Headache: A striking prodromal and persistent symptoms, predictive of COVID 19 clinical evolution. Cephalalgia. 2020; 40(13):1410-1421. doi: 10.1177/0333102410965157
- Tana, C, Bentivegna, E., Cho, SJ. et al. Long COVID headache. J Headache Pain 23, 93 (2022). https://doi.org/10.1186/s10196-022-01450-8
- Pazdro-Zastaweny K, Dorobisz K, Misiak P, Kruk-Krzemien A, Zatonski T. Vestibular disorders in patients after COVID 19 infection. Front Neurol. 2022 Sep 20;13:956515. doi:10.3389/fneur.2022.956515. PMID: 36203969; PMCID: PMC9531925
Meet marina, founder of parent with migraine
Learn how to approach parenting with chronic illness to tackle high symptom days, address parenting guilt and find acceptance with founder of Parenting with Migraine, Marina Medved-Lentini. Through her own personal experience she has created a platform to offer support, resources and guidance for other parents facing similar challenges.
Website is: here or you can copy and paste into your browser: https://parentingwithmigraine.com/
Instagram: @parentingwithmigraine here.
Marina has been living with migraine disease throughout her life. Her migraine attacks were episodic during her teenage years and through college and law school. After becoming a parent, Marina began to experience chronic migraine. Finding migraine support groups on social media helped Marina find hope, support, and information to work with her medical team to get her migraine managed. Her experience has motivated her to share her knowledge with others and become a migraine advocate. In vestibular group fit, Marina and Dr. Madison talk about screen time, parent guild, ways to prep and adapt when parenting with chronic illness.
Parenting with Chronic Illness Tip: Parent Guilt
Parent guilt can come in feelings of inadequacy, guilt of missing out on precious moments, or not feeling present or providing enough for your family. We tend to be our own biggest critic, and it’s important to look at these thoughts and feelings to determine what might be stemming from self doubt or own inner critic.
Having a chronic illness doesn’t define you. Parenting with chronic illness doesn’t define your value as a parent. You are strong and your provide your own set of strength and perspective as a result of your lived experience, chronic illness included.
Tips to help combat parent guilt:
- don’t compare yourself to others. social media can create unrealistic expectations. If your kids are happy and have what they need, that’s what matters! Marina shares her realization that kids want to feel included in your life and this can be done with simple connections like watching a movie together. It doesn’t have to be an elaborate social media activity.
- be kind to yourself. What would you say if this was your best friend having thoughts of self doubt? Is that what you’re telling yourself, or is your harsh inner critic talking?
- Doing your best is what counts. It’s okay to ask for help. If friends or family have shown interest in helping, take them up on it. A little help can go a long way.
- Get support! finding a community of those who share similar experiences and struggles can create a space to share openly your thoughts and feelings. You’re not alone in this.
Sometimes parent guilt comes in the form of potentially passing on a chronic illness such as migraine to your child. Migraine disease does have a hereditary component. Knowing about the signs and symptoms of your chronic illness in children can help identify the need for intervention quickly. Remember, there is so much more to a child than a chronic illness. Kids are resilient and have repeatedly reminded me that there’s something to be excited about and get the most out of life.
In the case of pediatric migraine, Marina shares resources on learning signs and symptom of migraine in kids to help get them proper resources. Migraine at school is a great resources for parents, educators and how to help support students. check them out here!
Parenting with chronic illness tip: preparedness and adaptability
Part of parenting is having to be flexible and adapt to changing situations. This is even more true when parenting with chronic illness. Having some items prepared can help on days when you’re not feeling your best. check out some tips below.
- Talk to your children about your chronic illness. It doesn’t have to be super in depth, but at a level they can understand. Answer any questions they have. Being honest with your kids can help them understand more of what’s going on if you’re not feeling well, instead of potentially catastrophizing the situation into a worse case scenario in their minds.
- As kids get older, they may benefit from having a role to help support you. This might be grabbing an ice pack or a migraine kit for you. Maybe it’s brainstorming a list of activities they can engage in more individually or next to you that are better tolerated when you’re not feeling your best.

Parenting with chronic illness tip: acceptance
Finding acceptance and self compassion has been noted by many as a main part of living with a chronic illness. Acceptance doesn’t mean you’re giving up but learning to live with a chronic illness. This includes finding ways for best management while coming up with solutions to keep doing your everyday. Your plan for you day might change or look completely different than you expected and that’s okay! Acceptance helps us address the stress and change of the unknown. We cover this more in our self compassion blog and premium content in vestibular group fit and more on acceptance in this blog post.
Disclaimer
Want to learn more about how to parenting with chronic illness, household tasks and social situations and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.

