Inflammation and dizziness
Have you tried traditional treatment for your vestibular condition or dizziness but feel like somethings missing? Dr. Emily Kostelnik discusses how unlocking the connection of inflammation and her body helped her find the missing piece of her vestibular treatment and management.
Meet Dr. Emily Kostelnik, PHD
Dr. Emily’s vestibular story
Dr. Emily Kostelnik is a clinical health psychologist and has her own personal experience with vestibular orders and dizziness. She has combined her personal and professional experience to assist others with vestibular conditions through Rooted Behavioral Education (link here) and her practice as a clinical health psychologist The Vestibular Psychologist (website here)
Follow her on instagram at rootedbehvaioraleducation and thevestibularpsychologist. She’s a wealth of knowledge and shares this on her social media accounts!
Dr. Emily also has a course on fucntional medicine, inflammation and alternative answers to dizziness. You can purchase the course here. Vestibular Group Fit members get a $75 discount so look in your premium content, or sign up for the discount ( you still save $15). If you’re unsure if this discount code is still active, email us and ask prior to purchase!
Dr. Emily Kostelnik was diagnosed with Superior Canal Dehiscence (SCDS) in 2018 with two surgeries to correct. In post partum, Dr. Kostelnik faced debilitating PPPD and VM.
Starting with more conventional treatment (VRT, Heal your headache diet, working with an otolgist), she noticed progress but still noted lingering symptoms. Medications were prescribed to address ongoing floating sensations, trouble with screen time etc but she felt like there was still something missing.
With the assistance of functional and integrative medicine doctors, Dr. Kostelnik researched more the possible role of inflammation and dizziness. This turned out to be an important part of her recovery and management strategy and she’s here to share what she’s learned. Overall she is dizzy free most days!
Yes, Dr. Kostelnik is dizzy from time to time, but again, is mostly dizzy free!
What is inflammation?
To understand inflammation in our bodies, we need to talk about our immune system. Our immune system defends our body from outside threats. Think bacteria, viruses, pollen, infections etc. Anything our body finds suspicious or potentially harmful, our immune system attacks.
Inflammation is the immune system’s response to a threat. Not all inflammation is bad, it is the first part of the healing process. Initially inflammation is good! It helps identify and surround the perceived threat to avoid damage to other tissues or further spread. This is done by the immune system leaking fluid and protective chemicals to the specific area. Typically, the next step is to clean out this area of the threat, and the acute inflammation phase is over and our body starts the next phase of returning to baseline.
When our body doesn’t start the next step and stays in the inflammatory phase, this can lead to chronic inflammation. In chronic inflammation, our body continues to respond like there is a present threat. A persistent state of chronic inflammation can feel like a decline in our health, like you’re never feeling like your best self.
Chronic inflammation can be a result of: chronic injuries, chronic infections, surgical implants, things we eat, the way we act (or don’t act…mindset is important!), sedentary lifestyle, our environment. A certain combination of factors, everyone is different, can begin to overwhelm our bodies and we then reach a state of chronic inflammation.
How does inflammation and dizziness fit together?
Research has found that people with vestibular disorders (acoustic neuroma, vestibular neuritis, vestibular migraine, BPPV, PPPD) and those with anxiety depression were associated with higher inflammatory markers. Inflammation can affect us all differently. For some, it causes dizziness, for other it may be migraine or a thyroid condition.
If our body is inflammed, and constantly trying to remove a threat, it impacts our body’s ability to function. This is additional energy, resources and stress on our body dedicated to increased inflammation. When our bodies are in this state, it’s hard to reach baseline or feel like your typical self.
3 Ways to that can help improve inflammation
- Exercise can help reduce inflammation in our bodies
- nutrition. our gut biome is super important. Eating inflammatory foods or having guy dysbiosis can impact inflammation in our body
- mindset. working on positive thoughts, or being with others to get a positive mood boost can work wonders for our body!
Mast Cell Activation Syndrome, Histamine, inflammation and dizziness.
We won’t go into much detail here, but you can find more on this via Dr Emily’s social media and in the interview with Dr. Emily and Dr. Madison for vestibular group fit members.
Mast cells release chemicals when a threat is perceived. Mast cells release many different chemicals, one of them is histamine. Too much histamine in our body can result in histamine intolerance and can contribute to chronic inflammation.
There’s a wide variety of opinion on this subject, and diagnostic criteria can be hard to accurately measure and meet. Even if you don’t meet the diagnostic criteria, you may still benefit from different management options. Talk if over with your doctor.
What about medications, supplements, antihistamines for inflammation and dizziness or MCAS?
Medications
- We can’t tell you what to take, that’s a conversation for your doctor. We’re big fans of taking meds when you need it and if that’s something you want to take. Medications aren’t a sign of failure and don’t have to be a forever thing if you don’t want it to be. Again, this is a hugely important conversation to have with your doctor! If they don’t support your preferences on this topic, find one that does if you can!
- It will be trial and error to find a med that works best for you. Meds are just one part of the treatment pie so keep in mind those other treatment options.
- if you’re on a med and happy with your current plan, great! Keep doing what you’re doing
Supplements
- everyone is different, some may benefit from supplements, others may not.
- this is very person specific, what does your body need and what are the routes to get it?
Anti-histamines
- again, what works best for you?
- some find elimination diets can be helpful, but this is a SHORT TERM SOLUTION. This can help determine why cells get overactive, or discover if there’s a personal connection in histamines, inflammation and dizziness for you
- anti-histamines may help symptom management, but long term use can have other health consequences including increased risk of dementia, or increased production of histamines to counteract the long term blockage. Again, do what works for you, have these conversations with your doctor. This may be a short term solution to dig deeper and find a longer term management plan!
How to Find and Functional Medicine Doctor
Find a list of all functional doctors here at IFM.org.
Reminder, functional doctors may have differing opinions on what they think is going on, and course of treatment. It may take a few to find the right fit or find the help that works best for you! Some may be helpful for inflammation and dizziness, you may find them helpful for other health conditions you don’t feel have been fully addressed!
Disclaimer
Want to learn more about inflammation and dizziness, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
EFT tapping for dizziness
EFT or Tapping is a free and easy way to address unpleasant experiences, emotions, memories and you guess it, dizziness! EFT practitioner Rochelle Schulz dives into what EFT is, the benefits and how to do it anywhere.
Meet EFT practitioner Rochelle Schulz

Rochelle Schulz is an EFT practitioner offering internationally accredited and certified services. With a focus on trauma-informed training, she creates a safe and non-judgmental space for adult individuals worldwide, both in-person and online.
Rochelle’s goal is to assist clients in healing, personal growth, and regaining confidence. By delving into the subconscious mind, we uncover and release patterns that have been running in the background, including traumas, phobias, cravings, and physical pain. Working together, Rochelle’s clients can reclaim their authentic selves and experience a life of meaning, joy, and purpose.
Rochelle Schulz specializes in guiding clients through uncomfortable emotions and facilitating a smooth journey for their brain and nervous system, minimizing dysregulation.
Here website is linked here to learn more about Rochelle’s services and offerings. She assist with individuals, group sessions, creating scripts to use on your own tapping sessions, free consultations and more!
What is Emotional Freedom Techniques (EFT Tapping)
EFT or tapping has been around since the 1970s and involves tapping with your fingers on different pressure points on the body. These pressure points are the same ones used in acupuncture but without the needles. Rochelle notes that EFT is an effect strategy for stress relief, boost immune system function, and turn off genes related to chronic illness.
EFT combines the concepts of energy pathways (meridians) rooted in acupuncture with somatic and cognitive behavior therapy to calm our nervous system and address difficult emotions and memories.
It’s effective, can be done anywhere, anytime, and you can do it yourself for free!
What is Bottom up therapy?
EFT is a bottom up therapy. Typically, when addressing dizziness, emotions, trauma etc, therapies are focusing on the head/brain. The brain is important in our experiences, but our cognition only makes up 20% of that experience. Rochelle goes on to explain that the body stores up to 80% of our experiences and memories in 4 different ways. They are:
- emotional memory
- sensory memory (hearing, sight, taste, touch)
- autonomic memory (temperature, respiratory, digestion)
- physical memory (muscle memory or movement memory)
Bottom up therapy looks to address the 80% of experiences and memories stored in our body. To process and calm our nervous system in this way, bottom up therapy is looking to address the majority of our body that other interventions ignore.
How EFT Can Be Used
EFT/Tapping can be used on three different levels:
- First aid calm down: This is used in the moment of a stressful event (traffic, hard conversations etc).
- Taming the trigger: It can help us reduce the emotional intensity of triggers. This allows us to respond calmly in the moment when this trigger is enacted.
- Trauma release: EFT can address deep-seated beliefs and traumas from our past that may affect our self-perception and behavior as adults.
EFT aims to find the root cause of limiting beliefs or traumas and release them, allowing us to let go of old programming, retrain our brain to have positive neural pathways, and live more freely. EFT tapping for dizziness can help break the dizzy anxious cycle, find acceptance, and retrain our body/brain neural connections for long term results. This takes time and practice!
Common Accupressure Points used in EFT Tapping
Using one or both hands, listed below are acupressure points used in EFT/Tapping.
- Side of the hand between the bottom of your palm and start of your pinky finger
- eyebrow
- side of the eye (near the temple but want to be on the firm/bone part, NOT the soft part)
- under the eye
- under the nose
- chin/under the mouth
- collarbone
- under the arm (4 inches below the armpit). You can reach across your body to tap this area or use tap on the same hand/under the arm if it’s comfortable to you.
- top of the head
Considerations for EFT tapping for dizziness
Some find that areas by the eyes or peripheral vision increased dizziness. If you notice this, choose tapping points that feel best to you (collar bone, under the arms, top of the head etc). Sometimes eyes closed or laying down can help this as well.

How to do EFT Tapping for Dizziness
1. RANK THE INTENSITY
Rank the intensity of the issue on a scale of 0–10.
2. TAP ON THE SIDE OF THE HAND
Tap with 4 fingers the edge/palm of your hand, near the base of your pinky finger.
“Even though I have [insert emotion, symtpom etc] in [insert location in your body] when I think about this [feeling, memory, experience, situation], I deeply and completely accept myself.”
Allow your body to soften and relax, be present with any symptoms or discomfort. You can acknowledge sensations without needing to control them.
Thank your body for its effort to protect you and give yourself permission to receive instead of resisting.
3. TAP WITH REMINDER PHRASE
The reminder phrase should acknowledge the issue and convey self-acceptance in spite of it.
some examples are:
- I’m willing to allow these thoughts and emotions now
- I’m noticing what I’m feeling in my body
- I’m recognizing these symptoms
- I’m allowing to be with this discomfort/illness
- I’m going to tune in and be with these symptoms
- It can be scary sometimes. Even though I think I need to control this. I can still soften anyway.
- I’m thanking my body for trying to protect me in some way.
- I give myself permission to receive instead of resist; these sensations that are happening now.
Using two or more fingertips, tap approximately 5x on each point listed above for 1- 2 rounds while repeating your reminder phrase. This can change with each session, and pick the tapping points you feel best with. Avoid the ones that make you dizzy.
4. REASSESS THE INTENSITY
Rank the intensity of the issue on a scale of 0–10. Continue repeating rounds until the intensity reaches zero or plateaus.
Resources
The tapping solution has a website and a smartphone app to help learn and perform guided tapping sessions. There’s a free and paid version! Check it out here.
Work with Rochelle Schulz! She has individual, group and free consultation services. Check out her website here.
Disclaimer
Want to learn more about different benefits of various tapping points, a guided tapping session with Dr. Madison and Rochelle Schulz, other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
In Vestibular Group Fit, Dr Madison Oak and Vestibular PT Cheryl Wylie, MPT talk all things BPPV and vestibular migraine. They discuss what BPPV is, what assessment and treatment look like, and Cheryl’s amazing app Healing Vertigo (check it out here). There’s great conversation too revolving around a very common yet difficult task, am I dizzy with a vestibular migraine flare, or BPPV? Read on for some background, or jump to the differences between BPPV and VM at the of this post.
Cheryl Wylie has been working in vestibular rehabilation for 13 years. Throughout her time traveling, she realized how common BPPV is, yet how difficult it can be to get it treated for those outside of big cities and specialized therapists. The app Cheryl created, Healing Vertigo, is designed for patients to learn how to address BPPV themselves.
What is BPPV?
BPPV stands for “Benign Paroxysmal Positional Vertigo”. This is a common vestibular condition, and gets its name from its own characteristics.
Benign: Not harmful (Don’t worry, we know firsthand how disruptive, scary and down right uncomfortable BPPV is…we have had it! They used the term benign in naming BPPV due to the fact it is not considered life threatening.)
Paroxysmal: sudden onset
Positional: certain head/body positions bring on symptoms
Vertigo: sensation of motion or spinning
BPPV and the Vestibular System
We’ll keep this review brief, but feel free to check out this previous post that dives deep into all things BPPV here.
Our vestibular system has 3 semicircular canals. These canals are filled with fluid and sit at different angles. Their job is to detect angular motion (are we moving sideways, up, down diagonal).
In the otolith of the inner ear, tiny (but heavy for their size) crystals that help detect gravity and motion.

If a crystal breaks away from the otolith and finds it’s way into a semicircular canal, this is the start of BPPV. When this crystal moves through the semicircular canal, the crystal pushes the fluid of the canal at a different rate. Our inner ear is now sending two very different signals of movement to our brain to try and understand. This results in a specific eye movement called a nystagmus (more on this here). This is why testing involves certain head positions, and looking at your eyes to assess any nystagmus present. Nystagmus is important information in addition to head position to know the next course of action, treatment! Here’s a chart of the different nystagmus here.
NOT EVERYONE GETS DIZZY WITH BPPV. Some may not feel dizzy with BPPV, but off balance. This is why it’s important to screen for BPPV in those that are dizzy and those with balance concerns to rule out BPPV.
Vestibular Migraine
Vestibular migraine is a neurological condition that can result in a variety of unpleasant symptoms. Common symptoms of vestibular migraine include: brain fog, light/sound sensitivity, neck pain, tingling, vision changes, and dizziness and/or vertigo. For more background check out our beginners guide to vestibular migraine.
Those with vestibular migraine have most likely been treated for BPPV. The kicker here though, is not all had BPPV. Unfortunately, this results in people getting treated for BPPV over and over, with no change in symptoms or feeling worse than before. This is because vestibular migraine can result in positional dizziness, but is not due to BPPV. This is why it’s important to understand the mechanism and nystagmus of BPPV to determine if treatment is warranted, or if it is due to a vestibular migraine attack.
BPPV and Vestibular Migraine, which is it?
BPPV charactersistics:
- lasts 10-30 seconds typically (but can last longer if you have cupulolithiasis-read on here)
- nystagmus that matches a semicircular canal (chart here)
- Tends to have a slight symptom delay (a few seconds)
- will continue to happen until treated (spontaneous resolution can occur, but can take weeks and isn’t guaranteed)
Vestibular migraine characteristics:
- quick spins while sitting up or sensation of dropping
- nystagmus isn’t consistent. or doesn’t match that of BPPV
- comes with a migraine attack (light/sound/smell sensitivity etc).
- You feel like you keep doing the Epley and it doesn’t work
- You get episodes of spinning or dizziness in certain positions but will go away in a day or two without you doing any treatment and just “wait it out”.
It’s hard to know the difference between BPPV and vestibluar migraine. Hopefully this list helps point you in the right direction. BPPV needs to be treated with a repositioning maneuver to improve. A vestibular migraine needs to be treated during a flare, and then work on managing symptoms and increasing your migraine threshold. If you’re unsure, schedule with your vestibular PT for an assessment for BPPV or check out Cheryl’s Healing Vertigo App (website here, video presentation here)
Disclaimer
Want to learn more about what to expect with BPPV assessment and treatment, debu7nking BPPV myths, reducing BPPV risk and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Are you experiencing dizziness and struggling to pinpoint the root cause? Today we’re going to discuss how binocular vision dysfunction can be contributing to your dizziness, it isn’t always from your vestibular condition! In this blog post we well explore what binocular vision dysfunction is and why this can contribute to dizziness. Resources are included at the end to learn more and find a provider to see if treatment is right for you.
Binocular Vision Dysfunction with Dr. Eliza Whatley, O.D.
Vestibular Group Fit members are getting a 6 part video interview with Dr. Madison Oak, DPT and optometrist Dr. Eliza Whatley, O.D. These two get into what binocular vision dysfunction is, the different types, treatment options, and how to request accommodations at the eye doctor with a vestibular condition! In this blog post, we’ll cover what binocular vision dysfunction is, the different types, how binocular dysfunction and dizziness go together, and seeking treatment.
What is BVD?
Binocular vision dysfunction is when your eyes are misaligned, making it challenging for your body to interpret the input from the eyes to form 1 clear image in your brain. Binocular vision dysfunction can cause dizziness, headaches, and light sensitivity. The 3 main types of BVD are phorias, tropias and fusional vergence dysfunction.
What about when you go to an eye doctor and they say your eyes are fine but you aren’t convinced? They may be talking about accommodative disorders (blurry vision or astigmatisms). Binocular vision dysfunction goes beyond if your eyes are picking up clear images. Our eyes are positioned at slightly different angles; and binocular vision dysfunction can arise if we’re having trouble taking those two separate images (one from each eye) and forming one complete picture in our brain.
3 types of BVD
Phoria: If a phoria is occuring, the eyes are misaligned in their natural resting state. When your eyes have a target to focus on, this misalignment is not seen. This is identified with a cover uncover test. Your provider will cover one eye at a time and look for any changes in eye alignment when both eyes are no longer focusing on the same target.
Tropia: Tropias are also known as strabismus or eye turn. Typically the eyes sit in a deviated position and can be seen when looking at both eyes simultaneously. People with tropias tend to be more symptomatic because the eyes are having a hard time working together and focusing on targets.
Fusional vergence dysfunction: your eyes are aligned, but they are not working together.
How does BVD and dizziness go together
The VOR (vestibular ocular reflex) is the vestibular and visual systems working together to help keep images stable when we are moving. Having a vestibular disorder we rely more on vision to help with balance. If there’s an underlying issue with our visual system then it becomes more challenging to control vestibular symptoms (dizziness, imbalance, spinning sensations).
If our VOR is impaired both via vestibular and visual systems, this impaired VOR can result in bouncing eyes/nystagmus and reduce peripheral vision.
Vestibular conditions do no create vision dysfunction. Typically, people already have a binocular vision dysfunction but have learned to compensate for it and the dysfucntion is masked. Once a vestibular condition arises, the body has a more difficult time masking visual dysfunction. This can be due to the impaired VOR mentioned above, and the increased reliance on the visual system that is so common in those with vestibular disorders.
BVD treatments
Prisms. Prisms use different lenses to help move the image to a different location on the retina. This improves the position for image interpretation to reduce eye fatigue and double vision. Over time, your provider may adjust the prisms to gradual reduce the number of prisms needed for the desired effect. Some may no longer need prisms, some may need prisms as part of their glasses prescription, but are able to wean down the number of prism lenses over time.
Vision therapy and vision exercises. This is discussed in more detail with with 6 part interview provided to Vestibular Group Fit members. Below you can access resources to connect with a provider to help assess and determine exercises that are right for you. ….they exercise, check out VGF and find a provider/BVD Q to see what’s best for you.
Other Considerations
Other factors that can impact binocular vision dysfunction are accommodative disorders (trouble focusing on close or far objects). This is why it’s important to make sure your eye prescription is up to date.
Having light sensitivity? This can sometimes be due to a refractory issue call astigmatism. Make sure you’re letting your eye doctor know about light sensitivity so they can evaluate for this.
Are glasses or contacts are more helpful? This can depend on the type of binocular vision dysfunction. This is discussed more in Vestibular Group Fit!
Nervous about going to the eye doctor because of your dizziness? Ask an optometrist about different methods to get your eye glasses prescription than just flipping between lenses. They exist! Or ask to flip between lenses slower, or take breaks!
Other Resources
The Neurovisual Institute is a great resource for additional information: here’s some quick links below. Check out their homepage here for additional information on binocular vision dysfunction.
Find a provider here that can assist with binocular vision dysfunction and determine a plan with you.
Unsure if you have binocular vision dysfunction? Take the BVD-Q! This list of questions helps determine if you would benefit from BVD treatment and can help with finding a provider to assist.
Looking for first hand accounts? Check out Susan Barry! She wrote a book about her experience with vision therapy and includes the history and science behind vision. Check out her book or her Ted Talk on Youtube!
Join us for more at Vestibular Group Fit
Want to learn more about binocular vision dysfunction and catch the 6 part video interview with Dr. Elize Whatley? Check out Vestibular Group fit where there’s additional vestibular tools from the experts and you can be a part of a supportive community to get back to your daily life! Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Neck pain, dizziness, and what to do about it
Neck pain and dizziness is a common symptom that can have a significant impact on an individual’s daily life. It can also involve migraines, making it challenging to know where to start in finding relief. It’s important to address the root cause of the pain for long term relief and management. In this blog post, we will explore the connection between neck pain, migraines, and dizziness, and neck pain exercises.
How neck pain impacts migraines
The neck is made up of several small vertebrae, muscles, and ligaments that support the weight of the head. When these structures become injured or strained, it can cause pain that radiates to other areas of the body, including the head. Neck pain can be associated with migraine, either as a prodrome or interictal symptom. This can result in neck pain and dizziness, especially if you have vestibular migraine.
Some report feeling like their headaches start at their neck, or neck massages or stretching will set off a migraine. This lets us know that the neck is involved, and we want to continue with neck treatment BUT we need to be careful how much neck work is done at any given time to avoid setting off a migraine or headache.
Others feel like working on their neck helps improve their headache or relieves in entirely. This is great news and also tells us the neck is involved, but we can approach the neck in a different way, using neck pain exercises, stretches, manual work and other treatment options for symptom relief and long term management.
How neck pain impacts dizziness
Neck pain and dizziness are commonly paired together. When dizziness comes on, it’s natural for our body to tense up and try to limit head movements in attempts to reduce dizziness. Sometimes neck pain from an injury or tension adds to your body’s general stress and discomfort, amplifying overall discomfort and dizziness. There are also sensors in our neck that talk to our brain so we know where our head is in space. If these signals aren’t matching up with the other movement sensors in our body, or our brain is having a hard time integrating all this information, we can feel dizzy, bobble head like, spacey, and more.
Causes of neck pain
Neck pain can have many different causes, but some of the most common include:
- Poor Posture: Spending long periods sitting at a desk or slouching in a chair can cause tension in the neck muscles, leading to pain and stiffness. Poor posture doesn’t necessarily mean slouching, but just holding the same position for long periods of time. Poor posture for long periods can add additional strain on our muscles and make them work harder, potentially causing muscle strain and/or tension.
- Joint Laxity: Some of us are naturally more flexible than others. Sometimes this results in pain or discomfort from our joints because they don’t have as much support from our tendons and ligaments. Strengthening is important in these cases to build muscle tone and strength to help provide support. People with joint laxity feel may report the urge to pop or crack their joints for relief, or need to stretch. This relief is typically temporary.
- Movement Dysfunction: If the neck muscles and joints are not functioning properly, this can lead to pain and stiffness.
- Neck Injuries: Neck injuries, such as whiplash or sprains, can cause neck pain and dizziness. These injuries typically occur due to sudden movements or trauma to the neck, such as a car accident or a fall.
- Vestibular Disorders: a common statement I hear when working with those with vestibular conditions is head movements making symptoms worse. It’s natural for neck pain and tension to occur in those experiencing vestibular symptoms as your body tries to limit head movements.
- Arthritis: a natural part of aging and can result in neck stiffness and reduce mobility.
- Pinched Nerves: If a nerve is inflamed or crowded, it can cause pain, numbness, tingling.Neck pain can have many different causes, but some of the most common include:
- Poor Posture: Spending long periods sitting at a desk or slouching in a chair can cause tension in the neck muscles, leading to pain and stiffness. Poor posture doesn’t necessarily mean slouching, but just holding the same position for long periods of time. Poor posture for long periods can add additional strain on our muscles and make them work harder, potentially causing muscle strain and/or tension.
- Joint Laxity: Some of us are naturally more flexible than others. Sometimes this results in pain or discomfort from our joints because they don’t have as much support from our tendons and ligaments. Strengthening is important in these cases to build muscle tone and strength to help provide support. People with joint laxity feel may report the urge to pop or crack their joints for relief, or need to stretch. This relief is typically temporary.
- Movement Dysfunction: If the neck muscles and joints are not functioning properly, this can lead to pain and stiffness.
- Neck Injuries: Neck injuries, such as whiplash or sprains, can cause neck pain and dizziness. These injuries typically occur due to sudden movements or trauma to the neck, such as a car accident or a fall.
- Vestibular Disorders: a common statement I hear when working with those with vestibular conditions is head movements making symptoms worse. It’s natural for neck pain and tension to occur in those experiencing vestibular symptoms as your body tries to limit head movements.
- Arthritis: a natural part of aging and can result in neck stiffness and reduce mobility.
- Pinched Nerves: If a nerve is inflamed or crowded, it can cause pain, numbness, tingling.
Signs of possible neck involvement
The symptoms of neck pain can vary depending on the cause of the condition. Some common symptoms include:
- Neck Pain: The most obvious symptom of neck pain and dizziness is pain in the neck. The pain may be dull or sharp and can range from mild to severe.
- Headaches: Many people who experience neck pain and dizziness also suffer from headaches. The headaches may be located in the back of the head or around the temples.
- Dizziness: Some report sensations of their head floating, or not being connected to their head and body. These feelings may increase with head movements or neck pain.
- Numbness and Tingling: Pinched nerves can cause numbness and tingling in the neck and shoulders. This can be a sign that the nerve is being compressed and may require medical attention.
- Limited Range of Motion: Neck pain and stiffness can make it difficult to turn your head or move your neck freely.
Neck treatment options
The treatment for neck pain and dizziness will depend on the underlying cause of the condition. In some cases, the symptoms may go away on their own with time and rest. In other cases, medical intervention may be necessary. Some common treatments include:
- Exercise: Gentle stretching and strengthening exercises can help to improve neck mobility and reduce pain. It is important to consult with a healthcare provider to ensure that the exercises are safe and appropriate for each individual.
- Mindset Work: Chronic pain can often be exacerbated by stress and anxiety. Learning to manage stress through mindfulness practices or cognitive-behavioral therapy may help to reduce pain and improve overall well-being. Check out these recent blog posts that cover this more here and here.
- Movement and Posture: moving every 45 minutes and checking in on your posture is important to reduce muscle tension and strain.
- Migraine Management: Keep in mind other factors of your migraine treatment pie to reduce triggers and increase your threshold for symptom management.
Common neck exercises and stretches
Here are a variety of exercises and stretches that can help alleviate neck pain and improve mobility. Again, this can vary person to person based on the root cause of neck pain. This may assist with neck pain and dizziness, or reducing headache/mgraine frequency and intensity, or a combination of things. Listed below are common exercises used in neck pain treatment. Consult your doctor or physical therapist to make sure you’re cleared to exercise and finding the exercises that are best for you.
- Chin Tucks
- Rows. Here’s a video for home set up.
- Thoracic mobility work such as cat cows, thread the needle, and open books (laying down or upright in kneeling)
- Neck Stretches: Gentle stretching can help stretch the muscles in the neck and relieve tension. Check out this blog post that dives more into specific stretches with videos.
Neck pain and dizziness are very common and can come hand in hand. The exercises listed above can help relieve tension in the neck, shoulders, and upper back, which can reduce pain and improve mobility. It is important to consult with a healthcare professional before beginning any exercise program to ensure that the exercises are safe and appropriate for your specific condition. By incorporating these exercises into your daily routine, you can reduce neck pain and improve your overall quality of life
Want to learn more about neck pain, with example progression and exercise plans and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more below:
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
How to get through your ‘To Do’ List & Daily tasks with dizziness
Energy conservation (or pacing) is a way to listen to your body and strategize your day to get chores done while minimizing fatigue and dizziness as much as possible. Read on to learn how to get through your ‘to do’ list and daily tasks with dizziness, learn why it’s hard, ways to get it done today!
Phone battery analogy
Use a 0-100% battery meter to gauge your energy levels and dizziness on any given day. Keep in mind tasks you do will drain your batter, just like using your phone will drain it. Don’t let your energy battery (or phone battery) reach zero. It’s easier to charge when you’re at 70-80% than when you’re at 10%.
6 Tips & Tricks to pace with dizzness
Take a look at these 6 tips to strategize your day. Consider your energy/dizzy battery for the day and these tips to map out your day. Reminder, it’s okay to ask for help, to prep part of a task for a later day (like soaking dishes), or delegate to another family member or service.
Some days we have big plans to get things done, but we wake up with increase symptoms, fatigue, and a lower body battery. That’s okay, it’s not your fault and you are not a failure. Focus on what can be done, including self care to have the capacity for your list another time.

Household and daily tasks with dizziness: the breakdown
In this section we’ll cover some common household chores or daily tasks and discuss why they’re challenging and ways to make them easier.
Our premium content members also have guidance on movements and strength exercises to increase their tolerance to these tasks. Doing exercises and movement will make tasks easier to do in the future. Learn more here.
Dishes
Why it’s difficult:
- Repetitive body movement (from sink to rinse to drying rack)
- eye tracking
- standing balance
How to pace with dizziness:
- Use the dishwasher if available
- stack dishes to move more at once and reduce large/repetitive movements
- soak dishes to make cleaning easier and faster
- wash multiple items before rinsing to reduce movements
- try a suction glass cleaner to take some of the effort of off you.
Laundry
Why it’s difficult:
- lots of up/down movements
- busy visuals
- noise/smells/light depending on the environment
- mental energy to sort and fold
How to pace with dizziness:
- ask for help. Have family take their own pile of laundry to put away or fold
- do folding and sorting seated
- Make laundry your one task for the day. Break down the tasks to give yourself rest time
- don’t fold everything! I’ve started to keep clothes I don’t mind being wrinkly in fabric bins. When I sort laundry I can put my socks in the sock bin, delicates in the delicate bin, and workout shirts/shorts in their bin. Cuts down my laundry time and I realized how much folding I did for things that I didn’t care about needing to be folded.
Stairs
Why it’s difficult:
- physically demanding
- looking down
- visually challenging: seeing both near and far
How to pace with dizziness:
- Use the railing when available
- reduce trips by doing all tasks on the top floor and then going downstairs for tasks
- keep a basket at each end to place objects in that need to go up/down to avoid multiple trips. A great way to get others to help as well!
Cooking
Why it’s difficult:
- looking down
- balancing
- lots of turning and reaching
- tracking
- focus
How to pace with dizziness:
- use some prepped foods like pre cut veggies
- do food prep in sitting when able
- Find simple recipes, The Dizzy Cook is an awesome resource, her cookbook is here
- have some easy frozen and pre baked meals
- use a slow cooker
Computer time
Why it’s difficult:
- tracking and scanning
- head position and posture
- mental fatigue and concentration
- light sensitivity
How to pace with dizziness:
- ergonomics for better computer posture (some extra tips for set up here)
- avalux glasses (code: VERTIGODOC will you get $25 off) or other blue light blocking lenses
- taking breaks with the 20-20-20 rule
Reading
Why it’s difficult:
- mental fatigue and concentration
- tracking and scanning
- head position and posture
How to pace with dizziness:
- audiobooks when able
- use your finger to help track the line you’re reading
- take breaks
Showering, Grocery Shopping, Escalators, Elevators, the dentist/hair dresser, cleaning the house, gardening and more!
Learn why wall these tasks are challenging, ways to get these tasks done now and products that help, and how to work on movements to improve all of the tasks listed today! All of this and more is included in our supportive community at Vestibular Group Fit! Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Conquer vestibular migraine: a beginners guide
Here is a beginners guide to vestibular migraine. We’ll cover the difference between migraine, vestibular migraine, management tips and tricks, and when to start vestibular rehabilitation (VRT).
What is migraine? How is vestibular migraine different?
In general, migraine is a neurological disorder and has various symptoms that can be present. Here is a list of some common symptoms associated with migraine:
- head pain (typically experienced on one side, near the eye/temple region, but not always)
- vertigo, imbalance, and dizziness
- light sensitivy
- sound sensitivity
- smell sensitivity
- nausea/vomitting
- neck pain
- ear ringing/tinnitus
- visual changes
- tingling
- and more
Migraines act differently with each person. A common misconception is that a migraine is only a bad headache, or if you know someone with migraines and their symptoms are different than what you experience you think “oh well I don’t have migraines because they’re nothing like my friends”. If it’s impacting your life, it’s worth talking to a medical provider about!
Vestibular migraine
Vestibular migraine accounts for 3% of all migraines. This subtype of migraine has specific symptoms relating to the vestibular system (vertigo, imbalance, dizziness, brain fog, feeling “off”, lightheadedness etc).
The International Classification of Headache Disorders criteria for vestibular migraine are:
- At least 5 episodes of vestibular symptoms of moderate or severe intensity lasting 5 minutes to 72 hours
- Current or previous history of migraines with or without aura according to the ICHD classification
- One or more of the following migraine features with at least 50% of vestibular episodes:
-
- Headache with at least 2 of the following characteristics
- One-sided location, pulsating quality, moderate or severe pain intensity; photophobia or phonophobia
- Visual aura
- Not better accounted for by another vestibular or ICHD diagnosis
click here for the research article that outlines this criteria.
The big thing to remember here is that not all vestibular migraines have head pain/headaches. Headache can be present, as well as the other symptoms on the list above in addition to vestibular symptoms.
Phases of migraine
- There are 5 phases to migraine. Again, everyone can experience these phases differently, but are important to know to better identify how your body responds to a migraine event so you can act quickly when you begin to see signs of a migraine for best results.
The 5 phases are:
- Prodrome
- Symptoms that occur in the beginning of an attack. Can last hours to days
- Aura
- neurological symptoms that occur right before an attack. Can last 5min-60min
- Attack
- The most severe symptoms, lasting hours to days.
- Postdrome
- The end of an attack, gives you a “hangover” feeling. Can last hours to days
- Interictal
- Symptoms that are experienced between attacks (quick spins, fatigue, light and sound sensitivity are a few). This is due to the underlying migraine condition and where vestibular rehabilitation therapy (VRT) can be helpful. But it’s also very important to get the migraine under control before heading into VRT, more on this later!
When to start Vestibular Rehabiliation (VRT)
VRT is beneficial in addressing residual symptoms after migraine attacks, or the interictal symptoms experienced in day to day life. VRT is most effective when attacks are mostly under control. If you’re having multiple attacks in a month, or you’re having a hard time getting symptoms under control, VRT may not be appropriate at that time. A couple of sessions may be helpful for education to try various methods to get symptoms under control, or addressing neck pain through gentle stretching, manual work, postural and ergonomic education).
VRT is most beneficial when your migraine is under control. Using habituation principles to improve interictal symptoms is best done when your vestibular migraine is under control. If your migraine and symptoms aren’t well managed, trying to do VRT is like throwing gasoline on an already raging fire and hoping it burns out. This is why VRT can make you feel worse. It’s important to have a therapist familiar with vestibular disorders and vestibular migraine to guide and dose your VRT appropriately.
What should I do when I have a vestibular migraine attack
If you begin to feel an attack coming on, you want to initiate your plan as soon as possible to try to stop th eattack or minimze the severity or time of symptoms. This may look like:
- Acute meds prescribed by your neurologist
- magnesium
- ginger
- grounding and breath work
- gentle walking
- water
- electrolytes
- Cefaly or GammaCore
- essential oils
- icepack/headache hat
Vestibular migraine management
- Start with the basics:
- eating meals regularly
- consistent sleep
- hydration
- Gentle, daily movement
- Mindfulness and mindset work. Stress can be a big migraine trigger!
- Consider blue light glasses, ice packs/headache pack, educational books (found more in depth here)
- Research backed vitamins and supplements for migraine (full list here). Vestibular Group Fit members get 30% off their fullscript orders!
- Talk to a neuroglist to see if you fit a vestibular migraine diagnosis. Discuss a plan for you regarding preventative, acute and rescue medications.
- Track large symptom days to find patterns. (migraine buddy is a helpful app for this)
- Diet and hormones can also be involved. More on diet here and here and here; more on hormones here and here.
There’s a lot of great content on tis website for vesitbular migraine, I tried to include most of it here but might have missed some. Vestibular Group Fit is a great place to find all this information presented to you in one spot with excellent resources, with a community of others to provide their own experience, advice and guidance for symptom management, lifestyle changes, and support with movement.
Disclaimer
Want to learn more about vestibular migraine management and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
3 ways Somatic Therapy can help dizziness
Learn how somatic therapy can help dizziness with psychotherapist Kate Schwab, LCSW. We’ll cover what somatic therapy is, the benefits, and tools to get started today.
Kate Schwab, LCSW is a licensed clinical social worker and psychotherapist. In vestibular group fit, Dr. Madison and Kate talk about how somatic therapy can help dizziness and tools that are helpful in supporting your body.
What is Somatic Therapy
Somatic therapy combines psychology, neuroscience, ethology, physiology, indigenous healing practices, and medical biophysics. Guidance of somatic therapists assist you in learning what your body needs to feel supported.
3 parts of somatic therapy involve:
- Nervous system activation and overwhelm
- Pacing
- Support tools
We’ll take a look at each of these parts to learn how somatic therapy can help dizziness. More information and a recorded interview with Madison and Kate can accessed with a premium account.
How is Somatic Therapy different than Acceptance and Commitment Therapy (ACT) or Cognitive Behavioral Therapy (CBT)?
ACT/CBT are talk therapies type and focus on behavior. Both are symptom management focus. ACT brings in more mindfulness work: what are your behaviors and beliefs and changing those. With somatic therapy, it’s less symptom oriented and more of ‘what’s happening for you internally?’. We are looking at WHY those symptoms are there and deeper work. These areas cover different parts, so if you’ve had ACT or CBT therapy, you could benefit from somatic therapy. Keep reading to learn how somatic therapy can help with dizziness in its unique way.
Who could benefit from Somatic Therapy?
Most people can benefit from this work, and there are many reasons we experience trauma responses. Chronic illness can be traumatic and so in general somatic work can be really useful!
Nervous System Activation and Overwhelm
When first experiencing pain or dizziness, we begin to try everything and anything to make it go away. This urgency can lead to desperation, feeling overwhelmed and hyper vigilant of what we’re experiencing. This heightened state ramps up our sympathetic nervous system- the “fight flight or freeze”. This is not a state we are meant to be in for long periods of time,and normally kicks in when there is an external threat. When the threat is external, like a sudden loud noise or dark looming figure, this is extremely helpful to get us out of that area and to safety. In the case of dizziness, the perceived threat is internal, so how do we get to safety? This is where somatic therapy can help.
This is so so common in dizziness, check out this article on the dizzy anxious cycle and Dr. Emily Kostelnik with Rooted Behavior Education for more on this as well.
Back to how somatic therapy can help with dizziness. Learning how our own body and nervous system begins to ramp up and “activate” helps us identify what our body needs to get through these situations and move towards health and homeostasis. Everyone is different, and each situation is different.

If we ignore these signs, or don’t have the tools to help support what our body is telling us, we can reach a point of overwhelm and our body shuts down on us. Pacing is the practice of identifying these activations, and working on tools to assist your body, a major part of what Kate and other somatic therapists are amazing at!
Pacing
Pacing involves going SLOW. This is not easy and takes practice. This makes us think about the exact moment we are in and what our body is experiencing. Go into a quiet room and focus on moving towards health. Focusing on what you’re feeling right now, what your body needs right now. This is abstract and hard, which is why lovely people like Kate are here to help guide you further. Pacing helps identify what you’re experiencing, and getting support systems in place. This is how somatic therapy can help with dizziness.
Over time and with practice, the goal is you start to learn more about your body and have tools to support it. Pacing helps you be more aware of your window of tolerance. It’s okay to have nervous system activation, people like Kate help you to identify and work through it. If you aren’t in touch with your body, it’s hard to move along various activation states tolerably.

Support Tools, Avoiding Hyperawareness, Derealization/Dissociation
It’s important to check in with your body with chronic conditions and symptoms to avoid doing too much, making it easy to become hyper vigilant of what you’re feeling.
Try and know that you know how to handle this, and you’ve filled your prescriptions, and you can call your doc if needed, you have a support system, and at the same time you need to let your brain set it down and enjoy the moment that you’re in. This is hard and takes repetition and practice.
What about derealization or dissociation?
These come with the feeling like you aren’t real. Like you’re watching your world through a TV. Feeling disconnected or viewing the world from a glass plane. These can be survival mechanisms (and that’s not a bad thing!) but ways to try to shake this are:
- Breathing (box breathing or 4 counts inhale, 8 counts exhale. Hold briefly before repeating)
- talking out loud to yourself “I’m okay I am present, I am here”
- can you put on a podcast to laugh at, music to sing or dance to?
Give these a try, did it help? These are a few of the ways somatic therapy can help dizziness, derealization and dissociation.
Contact info
Follow Kate for ongoing education or reach out if you have questions or are interested in working with Kate to see how somatic therapy can help dizziness, chronic pain and more! Click here to reach Kate’s website.

Want to learn more about tools, how somatic therapy can help dizziness, and other vestibular tools to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
How mindset can improve dizziness
Is your dizziness causing a spiral of anxious, negative thoughts? Identifying these thoughts and reframing these feelings is how mindset can start to improve your attitude and outlook on your dizziness to get your life back.
Below we dive into why our thoughts are important and how reframing our thoughts to neutral or positive statements can create a cycle of healing, not a cycle of doom.
Mindset and critical thinking
Oxford dictionary defines critical thinking as “the objective analysis and evaluation of an issue in order to form judgement”. Taking the time to break down thoughts, we can decide if our thoughts need rephrasing to change our mindset. With practice, thoughts become more neutral or positive. The image below, courtesy of Brooke Castillo and The Life Coach School is a great reminder why our thoughts matter. Our thoughts produce feelings, which turn into action (or inaction), which gives us a certain result.
We have 60,000 thought per day, with many repetitive thoughts from the previous day or hours before. Combining practice and our brains ability to change over time (thanks neuroplasticity), our mindset can change and ultimately impact our actions and results.
This is how mindset can improve dizziness. Read on to learn frameworks, with examples, to get started today.

How does critical thinking and mindset help my dizziness?
For anyone that’s skeptical but still reading, let’s dive into mindset when it comes to dizziness. As discussed in previous posts, our brain wants to keep us safe. This is why the dizzy anxious cycle is so often intertwined. Here’s what typically happens:
- Our brain doesn’t know where we are in space and worries about our safety.
- To keep us safe our brain makes an “error signal” which can come in the form of dizziness, nausea, fogginess etc.
- We stop whatever we’re doing, very concerned and nervous about what just happened.
- This gives our brain a chance to figure out where we are in space, and those ill feelings begin to settle down.
Usually, this type of signaling happens with an outside threat (a bear, loud sudden noise etc). Feeling anxious is a useful feeling, but not when we get it doing laundry, dishes, playing with our children or trying to drive to work.
Taking time to pause, critically think and remind our brain that we are safe during our everyday tasks begins the mindset work that results in your ability to do more with dizziness, and keep your dizziness in check. Without this change in mindset, our body quickly spirals with anxiety, fear, and negative thoughts that can consume you and keep you from doing what you need.
Below are two frameworks with materials go help you use mindset to improve your dizziness.
Does this mean I need to be positive all the time?
NO. That is not the point of mindset work. It’s okay AND NORMAL to feel angry, sad, frustrated, anxious, scared. You’re allowed to have these thoughts and feelings. Allow yourself time and space to sit with these emotions and thoughts but don’t dwell on them forever. This is where mindset work comes into play. Give yourself time to process your emotions, then use mindset tools to progress forward and move on from these feelings. This takes repetition and practice. Fortunately for us, life is always throwing out new challenges, so there will be ample opportunities to practice. Mindset an improve dizziness, but also how we handle other challenges and stressors in our life as well.
Critical thinking frame works to try
The two frameworks we’ll go over today to practice how mindset can improve dizziness are:
- The Life Coach School’s Self Coaching Model by Brooke Castillo
- Switch Side Debate
One area to keep in mind here is not everything thought has to be positive. Neutral thoughts are still better than negative thoughts to get the benefits of mindset work. Examples of neutral thoughts are:
- Feelings are not facts
- with time and effort, I’m getting better
- I will have to try again
- I am okay today
- I’m doing my best today
- I am present
Let’s see how to put these ideas into action. Below are examples one can use for vestibular symptoms. Let us know what you think!
The Life Coach School Model
The example below uses Brooke Castillo and The Life Coach School handouts. This is a great resources to learn more, and have guided worksheets to practice.
The link for the self guided worksheet can be found here.
Here’s a handout from The Life School with more information regarding each section of the CTFAR framework in case you feel stuck.


The Switch Sides Method
This method is common practice for debates. This method can be a little easier to remember when first starting out, but the CTFAR framework gets easier to do with practice.
The switch sides method takes your first train of thought on how you’re feeling, write it all down. Then, write the exact opposite (feelings, thoughts, beliefs). Read both out loud. Which one is more helpful? Can you use the more helpful thoughts for your next steps/actions?

Reminder:
You get to choose your thoughts.
You can pick the helpful thought (neutral or positive)
You can break down your thought processes and challenge your thoughts.
Your brain needs to understand it’s safe before it can heal
Want to learn more about identifying and addressing negative thoughts, and other vestibular tools to get back to your daily life? Find out more at this below:
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
5 Main Audiology Tests for Vestibular Disorders
With vestibular audiologist Dr. Alexandra Smith, Au.D, CCC-A, F-AAA.
Dr. Alexandra Smith is based in Santa Fe, NM (you can find her clinic here) and works to identify, diagnose, treat and prevent various diseases, injuries or defects of the ear. Audiologists are also able to assist their clients with maintaining good hearing and can assist with hearing devices. Dr. Smith perform audiology testing for vestibular disorders and is going over them in more detail to help you better understand your test results and know what to expect. If you think you’d benefit from audiology testing for vestibular disorders, talk to your doctor about comprehensive audiology testing.
This blog post covers some content Dr. Smith covers with Dr. Madison Oak, vestibular physical therapist for our vestibular group fit members. These tests are common when evaluating for vestibular disorders but aren’t always well known or explained. Read below to learn more about audiology tests for vestibular disorders and what they can help tell you about your vestibular condition.
What is a vestibular audiologist?
A specialty within audiology which includes:
- Hearing and tinnitus evaluations
- Surgical implant care
- Vestibular evaluation
- Select vestibular treatments (like the epley maneuver for BPPV)
- Diagnostic tests which we’ll go into more detail below! (ECOG, audiogram, VNG, brain wave testing, positional testing and more)
Using audiology tests for vestibular disorders can be another piece of information to consider with other testing (MRI, physical therapy, occupational therapy, ENT, Neurology etc) to best determine a plan of care to manage your vestibular condition.
What is the role of a vestibular audiologist?
What does audiology testing and vestibular disorders have to do with each other? Anatomically, our inner ear has both a spatial awareness system (the vestibular system) AND hearing portions (the cochlea) that make up the inner ear. The nerve that connects our inner ear to the brain also branches from the same nerve to reach both of these sections. It is also common to have other ear symptoms or hearing changes with vestibular conditions, so it’s important to get testing done by a specialist in the hearing portion of our inner ear, an audiologist!

What are the 5 main audiology tests for vestibular disorders?
Common audiology tests for vestibular disorders include:
- VNG (Videonystagmography exam)
- Caloric testing
- ECOG (Electrocochleography exam)
- VEMP (Vestibular evoked myogenic potential)
- Audiogram
Below, we’ll go into more detail on what these tests measure, what to expect, and how these tests can help with vestibular diagnostics.
VNG (Videonystagmography exam)
- Goggles are worn to measure and track eye movements using special software and is tracked on a chart
- Wearing the goggles, the audiologist will perform an oculomotor exam (tracking targets, saccades/looking between multiple targets other eye movements)
- Positional testing such as the Dix hall pike (for BPPV testing)
- caloric testing, read on to learn more about this one
- VNG can help determine any positional dizziness like BPPV and identify any central signs that may warrant a referral to a neurologist, or peripheral signs that could point to a vestibular condition
Caloric testing
- Done with air or water, each ear gets 1 minute of warm and 1 minute of cool air/water
- The temperature of the warm and cold air/water is mild. This temperature change stimulates your vestibular system. This can cause uncomfortable sensations of movement or rotation.
- It is normal to feel dizzy for part of the test and it will go away. All you have to do is keep your eyes open!
- The stimulation of the vestibular system causes the dizzy sensation and eye movements (nystagmus- more on that here)
- These eye movements are being measured with infrared video goggles. The left and right ear are compared to see if the movements are symmetrical.
- If the left and right ear are asymmetrical, this could indicate a unilateral vestibular weakness or vestibular hypofunction (you can learn more about this here)
You are in control and can stop at anytime, it is NOT AN ATTACK.
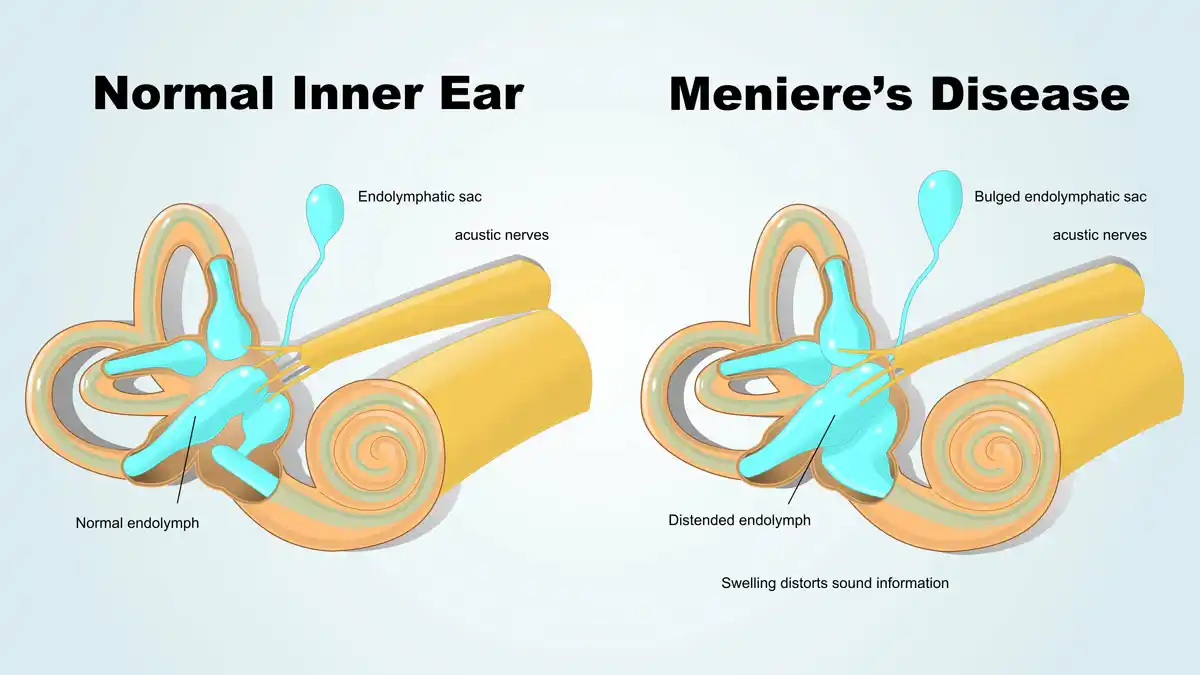
ECOG (Electrocochleography exam)
- A brain wave test that looks for increased fluid pressure in your endolymphatic sac in your inner ear (indicative of meniere’s disease)
- NOT a test in isolation of meniere’s disease-more accurate in the middle of an episode but more people don’t get into a clinic for testing during an episode
VEMP (Vestibular evoked myogenic potential)
- Cervical and ocular VEMPS are cVEMP or oVEMP
- Testing otolith function ( the utricle and saccule)
- Analyze the two branches of your vestibular nerve.
- Can see if one nerve is stronger than the other or if one side is weaker
- Can test for 3rd window syndrome like superior canals dehiscence syndrome
- Laying down on the table, one head movement and one eye movement.
Audiogram
- A hearing test, typically for first test you get in a audiologists office
- Can be very helpful in what’s going on and even help address what you’ve been experiencing
- Can tell you if you have hearing loss and where (what type of frequencies), and tympanic reflexes that can let us know about any ear pressure that man be going on
- Labyrinthitis will cause hearing loss
- Meniere’s disease also causes low frequency hearing loss on the affected side
- Age related hearing loss tends to be in both ears and at higher frequencies.
Can you have normal testing and still have a vestibular disorder?
YES! Certain vestibular conditions will not show up on this testing. Migraine will not show up on MRI, CT scans, ECOG VEMP or VNG or audiograms. These tests can still be helpful for these conditions that require a diagnosis of exclusion to rule out other conditions that these tests can reveal. Audiology tests for vestibular disorders can help lead us to identify specific diagnoses. If testing comes out normal, audiology tests for vestibular disorders can also help consider other diagnoses that would show normal testing.
Audiology tests for vestibular disorders is one piece of testing to be considered with other providers testing and listening to what you’ve experienced. Listening to your experience and looking at all the test results can help get the right team of providers (OT, PT, Neuro, ENT) in your corner to start your healing journey. It’s natural for this team to change slightly, or change focus for periods of time with certain providers based on your needs. Keep your team in the loop so they can help adjust accordingly, they’re here to help YOU.
Want to learn more about vestibular testing, ear pressure, tinnitus and other vestibular tools to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.