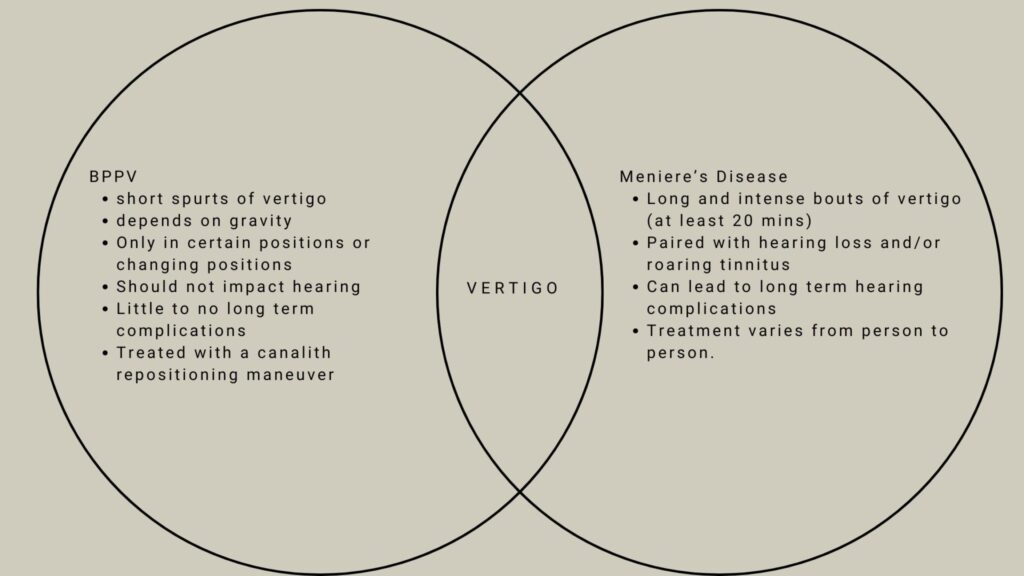
Vestibular disorders can be frustrating and complex, but they are all actually incredibly different. There are a few key factors that differentiate each from one another very distinctly. Two very distinct, but often confused, diagnoses are BPPV and Meniere’s Disease. Remember, BPPV stands for Benign Paroxysmal Positional Vertigo. The differences lie in the diagnostic criteria, as well as the clinical presentations. Both do come with room-spinning vertigo, but they will feel very very different.
Diagnostic Criteria
These two diagnoses are very different. BPPV will cause short and spontaneous episodes of vertigo, while Meniere’s Disease triggers long and difficult to tolerate episodes of vertigo.
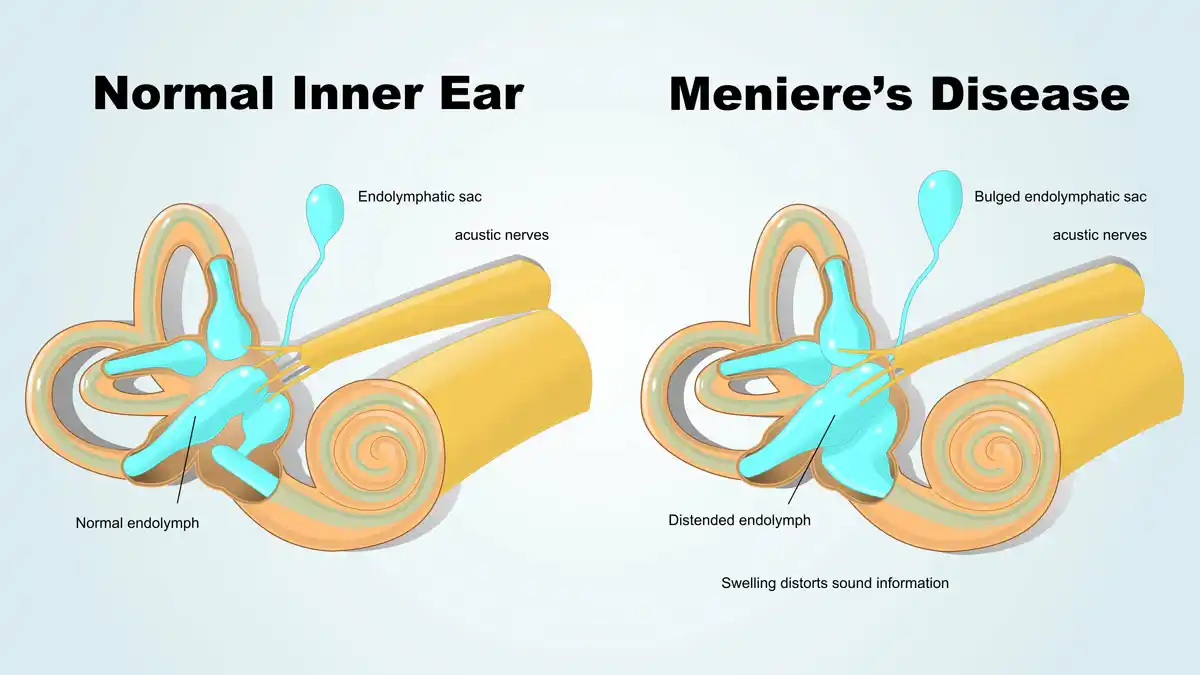
Meniere’s Disease (MD) Diagnostic Criteria:
- Two or more spontaneous episodes of vertigo each lasting 20 minutes to 12 hours
- Audiometrically documented low- to medium frequency sensorineural hearing loss in one ear, defining the affected ear on at least one occasion before, during or after one of the episodes of vertigo
- Fluctuating aural symptoms (hearing, tinnitus, or fullness) in the affected ear
- Not better accounted for by another vestibular diagnosis (1)
This is important to understand because many people (and providers) diagnose Meniere’s Disease despite people not actually meeting these criteria. This is especially try of my patients who tell me they have MD but have never experienced room spinning vertigo, or they experience quick spins, rather than long duration spinning, but still have an MD diagnosis. Those things do not qualify you for an MD diagnosis. So, when you may be thinking you may have this diagnosis, know that is both rare and requires a LOT of room spinning vertigo.
Speaking of being rare, yes, Meniere’s Disease is really rare. According to the American Hearing Research Foundation, only about .2% of the US population has Meniere’s Disease, where as BPPV is much more common (2). BPPV has a lifetime prevalence of 2.4%, meaning it will happen in about 2.4 % of the population at some point in their in their lifetime. That is WAY more than Meniere’s Disease (3)!
Benign Paroxysmal Positional Vertigo Diagnostic Criteria
A. Recurrent attacks of positional vertigo or positional dizziness provoked by lying down or
turning over in the supine position.
B. Duration of attacks < 1 min.
C. Positional nystagmus elicited after a latency of one or few seconds by the Dix-Hallpike maneuver or side-lying maneuver (Semont diagnostic maneuver). The nystagmus is a combination of torsional nystagmus with the upper pole of the eyes beating toward the lower ear combined with vertical nystagmus beating upward (toward the forehead) typically lasting < 1 minute.
D. Not attributable to another disorder.
Okay let’s break these down, because they’re a bit more confusing than the Meniere’s Disease diagnostic criteria.
What the BPPV criteria are saying is that when you lie down and sit up, you will have spontaneous room-spinning vertigo for less than 1 minute, which also has a delay (typically 5-10s) because it sets. AND it needs to be non-attributable to another disorder. This is where things get sticky, because vestibular migraine can actually act JUST like BPPV. I see people almost weekly in my clinic that say ‘I have been doing BPPV maneuvers for weeks, and NOTHING is happening,’ and it’s almost always actually vestibular migraine. To learn about the differences between vestibular migraine and BPPV, please click here.
So, how do I know the difference Between Meniere’s Disease and BPPV?
The best, and easiest, way to know the difference is based upon the length of your room spinning vertigo. If your vertigo is quick, and ends in less than a minute, it’s more likely to be BPPV (unless, of course, it’s VM, please read here). If the vertigo is more arduous, tiring, lasting longer than 20 minutes, but also causing hearing loss and tinnitus, it’s more likely to be Meniere’s disease.
What do I do if I have BPPV or Meniere’s Disease?
If you have BPPV, the best plan of care is to call your local physical therapist (hopefully a vestibular therapist!) and get in for a canalith repositioning maneuver to move the crystals back to where they belong! Out of your semicircular canals, and into the otolith organs.
If you have Meniere’s Disease, be sure to call your local vestibular ENT to talk about your treatment options and look further into why your body may have triggered this. There are definitely treatment options for you!
No matter what, there are treatment options for BPPV, MD, and VM. We have treatment options in Vestibular Group Fit, or you can find them at your local doctor. Be sure to address: the actual disorder, inflammation, lifestyle, blood work, and more! If you have questions about what these things should be, please reach out and join us here!
Sources:
(1) American Academy of Audiology. (2022, January 14). Classifications of meniere’s disease. https://www.audiology.org/classifications-of-menieres-disease/
(2) Meniere’s disease. American Hearing Research Foundation. (2022, August 24). https://www.american-hearing.org/disease/menieres-disease/
(3) von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007 Jul;78(7):710-5. doi: 10.1136/jnnp.2006.100420. Epub 2006 Nov 29. PMID: 17135456; PMCID: PMC2117684.
Vestibular disorders, which affect the inner ear and brain’s balance systems, can significantly impact a person’s quality of life. Identifying and managing triggers is essential for those dealing with conditions such as vestibular migraine (VM), Vestibular Neuritis (VN), Meniere’s Disease, and persistent postural-perceptual dizziness (PPPD). Below, we explore common triggers for vestibular disorders and strategies to minimize their impact.
First, we need to discuss the differences between triggers and causes. The CAUSE of a disorder is much different than its trigger. For example, the cause of vestibular migraine is a genetic predisposition to migraine, while the cause of an attack could be stress or too much stimulation. the cause of vestibular neuritis is a viral infection in your inner ear, whereas a trigger for the symptoms could be being in a busy environment for too long. Today, we are talking about triggers for increased symptoms and attacks, rather than the causes.
Common Vestibular Disorder Triggers
1. Stress and Anxiety
Stress and anxiety are leading triggers for vestibular symptoms. They can worsen dizziness, vertigo, and imbalance due to the brain-gut axis and its influence on the vestibular system. The more stressed you are, the worse dizziness gets, and the worse dizziness gets the worse anxiety and stress can become! To manage these requires both managing the dizziness as well as the anxiety/stress. We call this cycle the dizzy-anxious-dizzy cycle, and it can be broken with the right tools!
Management Tip: Regular mindfulness practices like meditation, deep breathing, and cognitive-behavioral therapy (CBT) can help reduce stress-induced vestibular flare-ups.
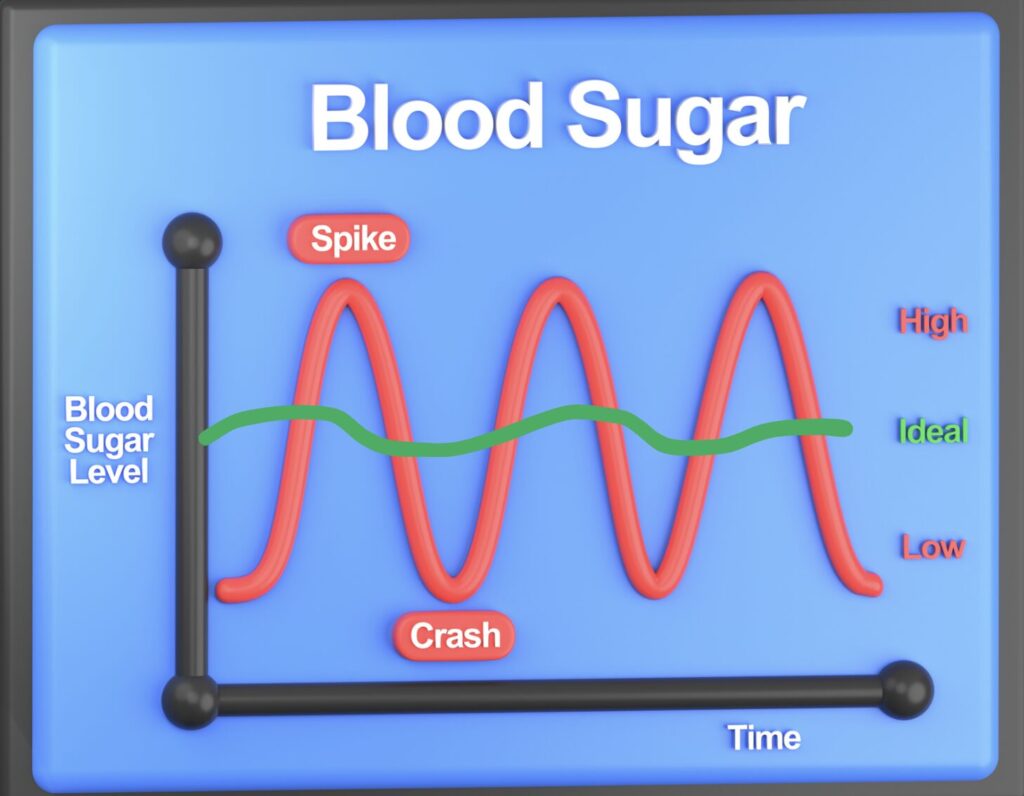
2. Certain Foods and Drinks, and an Imbalanced Blood Sugar!
Specific foods and beverages, particularly those high in histamines or containing caffeine and alcohol, may exacerbate vestibular symptoms. Processed foods and artificial sweeteners are also common culprits.
In addition to this, it’s also SUPER common for people to get attacks when their blood sugar is uneven. We are meant to keep our blood sugar pretty even throughout the day, like the green line in the photo below, however most people’s blood sugar spikes and then dips frequently throughout the day, which will lead to attacks coming more frequently!
Management Tip: Keep a food diary to identify patterns, as well as a blood glucose monitor for a few weeks, which can be prescribed by your PCP.
3. Environmental Factors
Triggers such as bright or flickering lights, strong smells, loud noises, or crowded spaces can provoke vestibular symptoms, especially in vestibular migraine and PPPD. Remember, this is a bucket – the bigger you can make your bucket, the more easily you can manage your vestibular disorer. This is the concept and theory that we use in Vestibular Group Fit.
Management Tip: Use Avulux Glasses (code VERTIGODOC), noise-canceling headphones, Loops ear plugs, or avoid environments with overwhelming sensory input.
4. Sleep Deprivation
Inadequate or poor-quality sleep can exacerbate vestibular symptoms, including headaches, dizziness, and brain fog.
Management Tip: Establish a consistent sleep routine and ensure your sleep environment is optimized for restfulness (e.g., dark, cool, and quiet).
5. Weather and Barometric Pressure Changes
Changes in barometric pressure, particularly during storms, can trigger symptoms in vestibular migraine and Meniere’s disease patients. We love to recommend Weather X Ear plugs and its app which goes with it. This is because it will help you pinpoint when the weather is going to change and how to better regulate the pressure in your inner ear!
Management Tip: Monitor weather patterns and plan activities accordingly. Some patients find relief with pressure-stabilizing devices.
6. Head Movements or Position Changes
Sudden head movements or lying down in certain positions can provoke vertigo episodes in almost all vestibular diagnoses. To counteract this, we recommend re-learning how to move your head again! This can be done as a piece of a vestibular rehab protocol, or it can be done from Vestibular Group Fit in the “how to move your head again” module!
Management Tip: Work with a physical therapist or vestibular rehabilitation specialist to practice gradual head movement desensitization.
7. Hormonal Fluctuations
Hormonal changes, including those during menstrual cycles, pregnancy, or menopause, are common vestibular disorder triggers, especially for vestibular migraine warriors! We find that the inability to properly get rid of (detox) estrogen or other hormones can be a big issue. Targeted strategies like red raspberry leaf tea, extra protein, cruciferous veggies, and more can help!
Management Tip: Track hormonal patterns and discuss targeted interventions, such as magnesium supplements or hormone regulation therapy, with your doctor.
8. Exposure to Toxins or Chemicals
Exposure to mold, volatile organic compounds (VOCs), or other environmental toxins can worsen vestibular symptoms. This is especially true for individuals with sensitivities like mast cell activation syndrome (MCAS).
Management Tip: Focus on creating a low-tox environment at home by reducing plastics, avoiding scented products, and using air purifiers.
How to Identify Your Personal Triggers
Tracking your symptoms alongside potential triggers is the first step. Use a symptom journal or app to record:
- Date and time of symptom onset
- Activities leading up to symptoms
- Foods and beverages consumed
- Environmental conditions
- Emotional state
This process can help you and your healthcare provider identify patterns and develop a personalized management plan.
Do I Really need To Avoid All These Triggers?
The short answer? Nope, you proably do NOT need to avoid all of these all of the time.
If you went around avoiding all stress all the time, never eating anything that could possibly trigger you, slept perfectly, never moved your head, figured out the perfect strategy for your period, and more…. that would take over your whole life. I do not believe in this taking over your whole life forever. Taking away all these things can truly shrink your life – and I have sen it happen over and over again!
So, instead, what should you do?
Instead, I recommend building a bigger bucket. Yes, a bigger bucket. Think of your threshold for triggers as a big bucket. The bigger your bucket, the more triggers you can tolerate before it overflows. So, if you build yourself a bigger bucket, it will expand your life rather than shrink it!
How do we build a bigger bucket, you may ask? Well, that takes time and consistency with a few key points. First, be sure to balance your blood sugar, as as many nourishing foods as you can, socialize, sleep, exercise, breathe, take time for yourself, hydrate, and so much more! This can feel overwhelming at first, but by slowly adding these ach into your routine, rather than starting all at once, you will get there!
I see vestibular migraine warriors go from home bound or bed bound to walking around the block and going to their children’s weddings using this tactic – so yes it does work. And, it works better than most other things I’ve seen done in this space!
Want to know where we do this? Vestibular Group Fit, of course! The best place to be if you are a vestibular warrior, check it out here!
Vestibular Group Fit is crafted to offer you a personalized and holistic approach to managing your vestibular disorder—without breaking the bank. We’re here to support you every step of the way.
Final Thoughts on Vestibular Disorder Triggers
Understanding your vestibular disorder triggers empowers you to take control of your condition. By identifying patterns and making small lifestyle adjustments, you can significantly reduce the frequency and severity of symptoms. Remember to consult with a healthcare provider to create a comprehensive plan tailored to your needs.
With the right strategies, you can regain balance in both your body and life.
The Ultimate Holiday Gift Guide for Vestibular Warriors Has Arrived!🎁
The holiday season is a time for giving, and what better way to show love and care than by choosing gifts that truly make a difference? If you or someone you care about is navigating life with a vestibular condition, this curated list of thoughtful gifts is here to inspire you. Each item is designed to bring comfort, relief, and joy to vestibular warriors during the holiday season—and beyond!
We’ve also included exclusive discount codes and offers to make your holiday shopping even easier. Let’s dive in!
1. Rise Centered Alarm Clock
Start the day with ease and calm. This sleek alarm clock is designed to minimize stress and help you wake up gently. Plus, it’s. absolutely 100% the MOST beautiful alarm clock I’ve seen in my entire life. Check it out!
💡 Holiday Offer: Get 10% off all clocks—or grab an “imperfect” clock for just $119! Offer Valid November 21-27, 2024 only!

2. Weighted Vest & Weighted Blanket
Grounding and calming, these weighted items are perfect for relieving anxiety and creating a sense of balance and security. I love the weighted vest for improved proprioception while doing activities around the house or going on a walk, but also for improving bone density! I love the weighted blanket for when patients are feeling a little under the weather, floaty, or bouncy; this blanket helps with grounding!
3. Stainless Steel Pots & Pans
Cook up something healthy and delicious with these nontoxic cookware essentials—great for reducing exposure to harmful chemicals. Non-stick pans can be toxic to the air you breathe when you’re cooking on them, and also can leach chemicals into your freshly cooked meal! Stainless steel helps us avoid this! While you’re at it, ditch your plastic spatula, too!
4. Ruhewell Dizzy Box & Grounding Bracelet
A thoughtful bundle designed specifically for vestibular health. The Dizzy Box is my tried and true box compilation of Ruhewell products. But, if you’re stocked up on those already, try Jill’s newest product that we collaborated on! The Graceful Grounding Bracelet, 30% off right now with Code VERTIGODOC at checkout! I loveee these because you become your own personal oil diffuser. I am highly highly sensitive to smells, and these don’t bother me a bit!
💡 Holiday Offer: Use code VERTIGODOC for a discount!

5. Stainless Steel Water Bottle
Stay hydrated with a durable, eco-friendly water bottle—because hydration is key to managing vestibular symptoms. If you’re even mildly dehydrated (which 75% of Americans are!) you will have more symptoms of dizziness! In fact, some studies have shown that if you dehydrate an athlete who is highly athletic and agile, and doesn’t have a concussion, they will perform with concussion-like symptoms! Stay hydated, friends! And, use stainless steel, it’s just superior!
6. Relief Band & Emeterm
Wearable relief for nausea and dizziness, these are must-haves for vestibular warriors on the go. I personally love these bands, and know that many of my patients do, too! I wear relief band on long car trips as well as on plane rides with turbulence. They work by stimulating and blocking the nausea signal to your brain! Check them out here!
7. Truvaga & Cefaly
Innovative devices designed to calm the nervous system and manage migraine symptoms—great tech for self-care. Cefaly is a trigeminal nerve stimulator, while Truvaga is a Vagus nerve stimulator. Both work a little differently from one another, and if you want to see what Cefaly looks like in use, check it out here!
💡 If you want a Cefaly for 15% off, use code VERTIGODOC at checkout!
8. Avulux Glasses
Specialized eyewear to reduce light sensitivity and migraine triggers. These have research proving that they are, indeed, the most superior of the glasses for migraine – nothing is better when it comes migraine glasses. They do have a return policy, so if you don’t love them in a few weeks, send them back (but I bet you won’t!).
💡 Holiday Offer: Use code VERTIGODOC for savings!

9. Ice Roller
A simple yet effective tool to reduce inflammation and soothe migraine pain. This one is tried and true. and, if I had to guess, I’d bet it’ll go on sale for Black Friday on Amazon.com! I am not joking when I say that I use this almost every single day. It doesn’t have to live in the fridge, it doesn’t melt everywhere, it’s easy to clean and it stays cold FOREVER. Get this one if you get an ice roller for you head!
10. Loops Ear Plugs
Noise and sound sensitivity is very real in this community and in the traumatic brain injury community. I have a cousin in a punk rock band who got in a car accident a few years ago. He never thought he’d play music again, but he can! He went to a lot of rehab, therapies, and so much more. But the one thing he never goes on stage without? Loops ear plugs. True story, friends! Grab a pair in any color – they’re amazing!
11. Mediterranean Migraine Cookbook
Filled with delicious recipes tailored for migraine-friendly eating, Alicia’s cook book is amazing. IF you’re looking to change your diet for migraine, a diet to su port your brain health is THE way to go – I recommend this focusing on eating mostly this diet and balancing your blood sugar over other diets for migraine. Yes, I said it, it’s the truth!
💡 Holiday Offer: Get signed hardback copies on Alicia’s site!
12. Vestibular 101
An easy-to-follow guide to understanding vestibular conditions. Dr. Emily K, Alicia Wolf, and myself made this course to focus on everything that Emily and Alicia wish they knew at the start of their vestibular journeys! You can find it all here, today, in one space, for just $84.15 through the new year, when the price goes back up to 99!
💡 Special Offer: Price already marked down—no code needed!
13. Vestibular Virtual Summit Replay
Vestibular Virtual Summit was MIND BLOWING for just about everyone who attended – myself included (…..and I organized it with Dr. Emily). It was THAT good. Revisit expert talks from the October 2024 summit, covering functional medicine and holistic approaches to vestibular care. If you’ve been curious about what’s next for you in your vestibular journey, this is it! WE talk about all the things your doctor probably forgot to mention at your last appointment (or what they might not even know yet!). Be ahead of the curve!
💡 Holiday Offer: Use code HOLIDAY for 15% off!
14. Work with Dr. Emily & Her Team
For personalized, holistic support, connect with experts in vestibular care at Rooted Behavioral Education. Dr. Emily and her team are absolutely excellent coaches and therapists. I have seen my patients thrive, reduce anxiety, and truly feel better working with Dr. Emily and her coaches! 💡 She’s offering $50 off her 1-off visits, and a discount on packages, too, through the end of 2024! Check her out here and mention you saw this offer from Dr. Madison for the discount!
15. Vestibular Group Fit Subscription
Vestibular Group Fit is crafted to offer you a personalized and holistic approach to managing your vestibular disorder—without breaking the bank. We’re here to support you every step of the way. Join a supportive coaching program designed to improve strength, balance, and resilience. There is no group like it, and nothing better to help you manage your vestibular disorder!
💡 Holiday Offer: Save 20% on your first cycle with code HOLIDAY!
What causes vertigo?
The Causes of vertigo are vast, but we first need to remember that Vertigo is a symptom, and never ever ever a diagnosis. Vertigo is like saying ‘it hurts’. What hurts? What does it feel like? Where is the pain? Is it sharp or dull? Is it acute or chronic? What is the cause of the pain, just like we would ask ‘what is the cause of the vertigo?’
Knowing the pain is like knowing your vertigo. It’s only a symptom, and it is never a diagnosis. We need to determine the cause of the vertigo in order to accurately help you understand your body better and manage life with a vestibular disorder!
What causes a vestibular disorder?
A vestibular disorder is an inner ear disorder that can cause many symptoms, including but not limited to, dizziness, vertigo, nausea, vomiting, lightheadedness, and more. Vestibular Disorders are largely split into central and peripheral vestibular disorders. A central disorder happens in your brain; like vestibular migraine, concussion, persistent postural perceptual dizziness, or a stroke. A peripheral vestibular disorder happens in the vestibular system itself, like vestibular neuritis, BPPV, or Meniere’s Disease.
In order to understand a vestibular disorder, we also need to understand the vestibular system itself.
What causes vertigo? Many things, but typically vestibular disorders are what causes vertigo.
What is the vestibular system?
Your vestibular system lives in your skull, deep in your inner ear. It is attached to your hearing organ, AKA your cochlea, and the vestibular system itself. It’s made up of bone, cartilage, and two types of fluid. If you want to learn more about the vestibular system and it’s inner workings, read more here.
5 causes of vestibular dysfunction
What causes vertigo? Vestibular disorders are very common causes of vertigo!
- Illness
- Injury
- Medication ototoxicity
- Mechanical issues and calcium debris
- Migraine disorders
Illnesses and infections of vestibular disorders
There are many illnesses that are associated with vestibular disorders, which cause vertigo symptoms.
Inner ear infections, like a vestibular neuritis, will leave you with a vestibular hypofunction, which is a peripheral vestibular disorder. IF you want to learn more about peripheral disorders, listen to this free podcast episode. This kind of inner ear infection can also cause labyrinthitis, which is the same as neuritis but includes hearing loss.
Long COVID is another infection that can cause dizziness. COVID infections can infect the vestibular system, also leaving you with a hypofunction, or can cut off the blood circulation to the inner ear, causing damage to the vestibular system itself. This can cause chronic or acute dizziness, both of which are treated in Vestibular Group Fit! You can read more about Long-COVID and dizziness in this article here.
Injuries and vestibular disorders
Your vestibular system can be injured, specifically with head and neck trauma, in a Traumatic Brain Injury. TBI, mTBI, or concussion can cause a vestibular hypofunction. In some cases, if the person is impacted in the side of their head it can cause a hypofunction in the vestibular system itself. These disorders, just like all disorders, are manageable and rewiring your brain with vestibular rehab is possible to do to get back to a place where dizziness is not 24/7.
Medication ototoxicity
Ototoxic medications are some NSAIDs, Chemotherapy drugs, Gentimicin, antimalarials, loop diuretics, and salicylates (1). Sometimes, these medications are absolutely necessary, especially chemotherapy medications. Because these medications can cause injury to the vestibular system(s), they can be what causes vertigo.
However, when they’re taken they can be toxic to your inner ear and cause a decrease in function, hypofunction, in one or both ears. This can cause intermittent or permanent symptoms in one or both ears. For example, after chemotherapy treatment, bilateral vestibular hypofunction can be common, as well as
Sometimes, there are intentional ototoxic doses of Gentamicin, like for the treatment of Meniere’s Disease.
Mechanical disorders and debris
Benign Paroxysmal Positional Vertigo, Superior Canal Dehiscence Syndrome, and Perilymph Fistula are all mechanical disorders.
BPPV is a mechanical disorder because calcium carbonate crystals are misplaces from the otolith organs into the semicircular canals, causing episodic vertigo. If you want to learn more about BPPV, click here.
Superior canal dehiscence and perilymph fistula are both mechanical disorders as they are physical holes in your inner ear causing specific symptoms. A surgical or other medical intervention is usually recommended.
Migraine disorders (Vestibular Migriane)
Migraine is more than just a headache. Migraine is a full body neurological disorder that occurs in your brain 24/7 but presents itself in attacks. Vestibular migraine is the most common cause of neurological dizziness and vertigo! Vestibular Migraine is so treatable, but can feel so difficult to get there. We will help you with this, as you need a comprehensive treatment program with a comprehensive outlook, from everything from medical treatment to lifestyle adjustments and being educated about your disorder.
Dizziness gets better, you just need the right tools!
The right tools exist and they’re all in 1 place in Vestibular Group Fit! You can learn more about Group, and why we use this method here.
Sources:
(1) Joo Y, Cruickshanks KJ, Klein BEK, Klein R, Hong O, Wallhagen M. Prevalence of ototoxic medication use among older adults in Beaver Dam, Wisconsin. J Am Assoc Nurse Pract. 2018 Jan;30(1):27-34. doi: 10.1097/JXX.0000000000000011. PMID: 29757919; PMCID: PMC6044447.
The vestibular system is a tiny system within the inner ear that is absolutely essential for our wellbeing. And just like all other parts of our bodies, things can absolutely go wrong. But, we can find ways to manage vestibular disorders, always! There is always always hope for dizziness, even chronic dizziness. Yes, really. Don’t believe me? Check out the Win’s page, called The Motivation to read through a few of the amazing success of Vestibular Group Fit members.
Movement stimulates the Vestibular System
Engaging in almost all activities, including but not limited to, pilates, strength training, yoga, tai chi, walking, running, dancing, or even simple head movements activates the vestibular system. As we move, the fluid in the semicircular canals shifts, triggering sensory hair cells that send signals to the brain. This continuous feedback loop is essential for spatial awareness, equilibrium, and overall coordination – in fact, moving in these ways actually strengthens these reactions. And, when we stop moving as much we will ended up with a weakened response system form the brain and vestibular system – we do not want that!
5 Benefits of Movement for Vestibular Health:
1. Improved Balance and Coordination
Your balance and coordination are essential to being able to walk, run, stand, ski, hike, and more. Just standing on a grassy surface rather than a concrete surface requires extra help. Regular movement challenges the vestibular system, promoting the development of better balance and coordination. This is particularly important as we age, as the risk of falls increases. It’s really a use it or lose it type of system. So, if you have a vestibular disorder and you’ve found yourself sitting still for long period, or any period for that matter returning to that same movement may prove difficult!
In Vestibular Group Fit, we will work with you personally to help you return to movement, and so much more. Join Here
2. Spatial orientation and Awareness
You know exactly how fast or slowly you’re moving, and we take that for granted. Same thing with your spatial awareness (so you don’t run into a door every single time you walk through a doorway, for example). Your vestibular system is responsible for so much of this, and is strengthened by getting yourself through busy environments. But, of course, there are difficulties with this if you have a vestibular disorder.
Whether navigating through a crowded space or participating in sports, an active lifestyle enhances our ability to perceive and respond to our surroundings. And, as you learn to live with your vestibular disorder, this will get easier. We just need to get you the right tools to thrive!
3. Exercise PREVENTS Vestibular Flares!
Yes, really. Vestibular disorders like Meniere’s Disease, Vestibular Migraine, Benign PAroxysmal Positional Vertigo, and more are managed with exercise. Yes, really. I know it feels so hard to believe, but there is evidence to show that all 3 of these diagnoses actually improve when you exercise. Migraine, specifically strength training, increases your migraine threshold and reduces migraine frequency and intensity. Walking is great, too! But it’s best when pared together. No, I don’t mean you should go all out on a marathon, but strength training and walking on a regular basis helps. If this sounds like you and you have Migraine, or any sort of chronic dizziness you NEED exercise, and we are here to help, in Vestibular Group Fit we will walk you through exactly how to do this and provide you the workout classes that will get you there!
4. Enhanced Cognitive Function:
So many people with dizziness and vestibular disorders reports brain fog or feeling fogged over. The best treatment for managing brain fog? Once again, it’s EXERCISE! Seems crazy, but exercise is preventative against brain fog and can really be a huge help. Research shows improved memory, cognitive function, and processing speed with a regular exercise routine. Don’t let dizziness stop you – start exercising, lift that brain fog!
5. Emotional Wellbeing
the dizzy anxious dizzy cycle is very very real. And, it need to be broken! There are a few things that we need to do to enhance this process, like challenging our thoughts (see: the critical thinking module in VGFit), and getting on a breathing schedule (see: The Basics in VGFit).
And, of course, we also need exercise. Exercising enhances neuroplasticity and improves the overall emotional wellbeing of all people who were on a regular exercise routine of all ages. And yes, this applies to you. Your body needs to move. As I sit here and write this article I am thinking about how I am going to move my body later in the day, and how I should be getting up right now. It’s SO much easier to sit still, that’s what our body feels most comfortable with, because it is made to conserve energy too. But, we are conserving too much, and not spending enough throughout the day (Even if you are fatigued!!). Your improved emotional wellbeing, from exercising (and everything else in Group Fit) will help you reduce the dizzy anxious dizzy cycle and help you break free of the chronic dizziness cycle.
You can break free from the dizzy anxious dizzy cycle. Whether you’ve dealt with dizziness for 1 day or 25+ years, it can be done!
Let me show you exactly how to do this, in the straightforward program that is Vestibular Group Fit. You don’t even have to start with movement if you don’t want to. There’s SO much to help you with your chronic symptoms.
Join us today!
Vestibular disorders & vestibular symptoms
The vestibular system, a remarkable and intricate network within our body. The Vestibular System plays a fundamental role in maintaining balance, equilibrium, and spatial orientation. Comprising various components, this system allows us to navigate the world around us with stability and coordination. The Vestibular System is your balance system, and it works with other body systems, specifically your proprioception and your vision, to keep you upright, track where you are in space, how fast you’re going, and more. If you have a vestibular disorder, any number of vestibular symptoms can occur, some of which may affect your balance and stability, while others may cause dizziness and lightheadedness.
The function of the Vestibular System
The primary function of the vestibular system is to provide the brain with information about the body’s motion and position relative to gravity. This sensory input is crucial for controlling our balance and coordinating movements. Essentially, the vestibular system serves as our internal gyroscope, constantly monitoring changes in head position and movement.
Imagine standing upright and tilting your head to the side—your vestibular system detects this change and signals the brain, allowing you to adjust your posture to stay balanced. Whether we are walking, running, or simply shifting our gaze, the vestibular system works seamlessly to ensure our body maintains equilibrium.
When something goes wrong with the vestibular system, that’s when we get vestibular symptoms!
1. Pieces of the Vestibular System
To comprehend the intricate workings of the vestibular system, it’s essential to understand its key components. It has quite a few pieces lined up together, and something can go wrong at any of the points in the system.
- The Vestibular System: The inner ear houses cochlea (your hearing organ) and the vestibular organs, consisting of the utricle and saccule, and three semicircular canals. These structures are filled with fluid and specialized sensory cells that detect head movements in all angles and directions. This helps us to best understand our spacial whereabouts and balance. Meniere’s Disease is a vestibular disorder that occurs in the vestibular system itself.
- Vestibular Nerve: The Vestibulocochlear nerve sends signals from the inner ear to the brain, the vestibular nerve plays a crucial role in relaying information about spatial orientation and motion. Things can go wrong here, like vestibular neuritis and Acoustic neuroma, for example. It connects the inner ear to the brainstem, forming a vital link in the vestibular pathway.
- Brainstem and brain: the brainstem processes and integrates signals from the vestibular nerve to the brain. the brain and brainstem coordinates reflexes, eye motion, gaze stability, posture, and more! Vestibular Migraine is the most common vestibular disorder that happens centrally (AKA in the brain and spinal cord)
2. Pieces of the Vestibular System
To comprehend the intricate workings of the vestibular system, it’s essential to understand its key components. It has quite a few pieces lined up together, and something can go wrong at any of the points in the system.
- The Vestibular System: The inner ear houses cochlea (your hearing organ) and the vestibular organs, consisting of the utricle and saccule, and three semicircular canals. These structures are filled with fluid and specialized sensory cells that detect head movements in all angles and directions. This helps us to best understand our spacial whereabouts and balance. Meniere’s Disease is a vestibular disorder that occurs in the vestibular system itself.
- Vestibular Nerve: The Vestibulocochlear nerve sends signals from the inner ear to the brain, the vestibular nerve plays a crucial role in relaying information about spatial orientation and motion. Things can go wrong here, like vestibular neuritis and Acoustic neuroma, for example. It connects the inner ear to the brainstem, forming a vital link in the vestibular pathway.
- Brainstem and brain: the brainstem processes and integrates signals from the vestibular nerve to the brain. the brain and brainstem coordinates reflexes, eye motion, gaze stability, posture, and more! Vestibular Migraine is the most common vestibular disorder that happens centrally (AKA in the brain and spinal cord)
3. Common Vestibular Symptoms
Vestibular Symptoms are often symptoms of imbalance and dizziness. These include, but are not limited to:
- Imbalance
- Vertigo (room spinning)
- Dizziness
- Light headedness
- Heavy headedness
- Gaze instability
- Internal Rocking and Swaying
- Feeling like you’re on a boat
- Difficulty walking in the dark
- Disorientation
Common symptoms that are also associated with vestibular disorders, but aren’t necessarily caused by the vestibular system itself:
- Anxiety
- Fear
- Depression
- Heart palpitations
- Agoraphobia
4. Triggers of Vestibular Symptoms
Vestibular symptoms come from many places, and triggers are never causes. The cause of your vestibular disorder will differ from the next person’s because some are caused by migraine disorders while others are caused by infection. Getting to the bottom of this will require opinions from vestibular physical therapists, neuro-otologists, neurologists, an ENT, and maybe even a headache specialist! Triggers will be different for everyone, of course, which means you will have different triggers than others. But, here are a few that can trigger flares or attacks:
- Excessive Light
- Excessive Sound
- Head motion (especially at first)
- Exercise (at first)
- Increased stress
- Anxiety
- Being sick
- Menstrual cycle
- Busy environments (like the grocery store)
- Travel
5. Should I avoid my Vestibular Symptom triggers?
This specific question is one of the most common, and the most complex. The short answer is no, don’t avoid if you can. However, sometimes we do want to avoid these triggers, too!
Avoiding your vestibular symptom triggers can come in handy sometimes. Specifically, if/when you are having a higher symptom day already, then avoiding triggers can be helpful. This is because if we do triggering activities while we are triggered and get even dizzier or more anxious, our body will continue to pair dizziness and fear with this specific task. The Grocery store is a great example here. If you are having a high symptom day when you wake up, for whatever reason, and then you go to the grocery store it’s likely you’ll get even dizzier. If this dizziness is triggered and makes you feel more anxious, frustrated, or fearful of the symptoms then it’s likely reinforce the dizzy-anxious dizzy cycle further into your brain. We want to avoid this. So, in this situation, it’s best to avoid the trigger. For more on this, I recommend the book The Way Out by Alan Gordon.
Otherwise, we want to try and engage with our active triggers in order to make it so they’re not so triggering for you. For example, if moving your head right and left causes symptoms, that is going to be something to not avoid. However, it is something you should work on with your vestibular PT in order to make this easier with time, avoid the fear and anxiety, and be able to ground yourself back to baseline between repetitions.
6. Treating your Vestibular Symptoms
Proper treatment of your vestibular symptoms is a comprehensive process, it requires a few different steps and providers. There is no single best option that exists for everyone, rather a few things all piled up together to create your personal treatment pie. This not only involves getting opinions from different providers and programs, but also requires us to remember that we need to know what each provider does so we can ask for the right thing.
Medical treatments for Vestibular Symptoms
Your medical doctor’s job is to provider you with medical treatments. This can be medications, supplement recommendations, testing, and referrals to other providers. Medications and medical treatments exist for Vestibular Migraine, Meniere’s Disease, Acoustic Neuroma, Superior Canal Dehiscence Syndrome, MDDS, and more. However, diagnoses like Vestibular Neuritis do not require medical treatment as much as they require physical therapy and mindset work.
Testing if you’re dizzy should consist of brain imaging (MRI/CT), a videonystagmography exam (VNG), other vestibular testing (like an ECOG, VEMP, etc.). You could also get bloodwork to see if you have any deficiencies.
Surgical treatments for Vestibular Symptoms
Some treatment protocols for certain vestibular disorders need surgery. Diagnoses like Acoustic Neuroma, Meniere’s Disease, and Superior Canal Dehiscence often call for surgical intervention. Be sure to interview a few surgeons before you determine which is best for you.
Physical treatments for Vestibular Symptoms
Vestibular Rehabilitation Therapy is often a great treatment for vestibular symptoms! A Vestibular Rehab Therapist will help you by figuring out your goals and working towards doing them without dizziness. a Vestibular Therapist can help you return to exercise, reduce visual vertigo, improve your balance, and more!
The most comprehensive treatment plan for Vestibular Symptoms
The most comprehensive treatment protocol you can get is always the best one. This will help you cover all your bases, raise your vestibular threshold, and be the least dizzy possible. This needs support and consistency. The best way to go about this is joining Vestibular Group Fit. VGFit is the comprehensive group program dedicated to helping you feel better. We work through the pillars of movement, mindset, support, and education. This program helps members feel better, less dizzy, and finally have freedom over their vestibular symptoms!
Want to finally feel better? I want that for you, too!
and we can get you there! Join us in Vestibular Group Fit today!
What is a vestibular disorder?
Vestibular disorders can have a profound impact on an individual’s daily life, affecting their balance, spatial orientation, and overall sense of well-being. In this comprehensive guide, we will delve into the intricacies of vestibular disorders, exploring their causes, symptoms, and various treatment options. Whether you’re experiencing these challenges firsthand or seeking information for a loved one, this article aims to shed light on this often misunderstood condition.
What is the vestibular system?
Your balance and equilibrium sensation is a whole body experience. Your Vestibular System is a massive piece in this puzzle, and when something goes wrong with it, imbalance, dizziness, vertigo, disequilibrium, and a general feeling of being ‘off’ ensues.
But what actually causes this? What is the vestibular system? Where does it live? And why in the world does this tiny, pea-sized, organ matter so much? In order to understand the dysfunction, we first must understand the system itself. Let’s dive in below! But, if you prefer to listen to anatomy and physiology, here’s a podcast episode about that.
Anatomy and physiology of the vestibular system:
The vestibular system is a very small, truly pea sized, organ that lives on either side of your head, deep in your skull. It is technically in your inner ear, which is the third and final ‘layer’ of your ear anatomy.
Your first have your outer ear. The outer ear is the part you can see and touch. It is from the big part that is on the outside of your hear, to the ear canal, ending at your ear drum, AKA the Tympanic Membrane. Your ear drum separates your outer ear from the middle ear.
Your middle ear is basically a balloon filled with air, regulated by the ear canal called the eustachian tube. The eustachian tube, in the photo below, is the piece that looks like Florida (I mean really, it does!). That piece is closed at baseline, but opens and shuts when you pop your ear. Your ear is supposed to pop, that’s normal! It helps you regulate the pressure and volume of the amount of air in your inner ear at any given time. Within the balloon piece of the inner ear are also the 3 tiny bones called the malleus, incus, and stapes. These three bones knock against and vibrate on each other to help send sound, in the form of vibration, to your inner ear. This is a big part of how we hear!
Lastly, we have the inner ear. The inner ear organ is made of two distinct parts of the same organ. The curly cue part that looks like a snail is your cochlea. The cochlea you likely learned about in biology class in high school and didn’t think much of again. probably until now! Because, why would you, so long as it works? Sound waves enter into the spiral and go a certain distance depending on if they’re high or low sounds, which are then communicated to your brain via the vestibulocochlear nerve. More on that nerve later!
The second part of your inner ear is the part we really care about in this little chat we are having today. That is your vestibular system. Your vestibular system is amazing, and is made up of two parts. Most people have never heard of it, or thought about it, until something goes wrong. And you’re not alone! there are two parts in here.
In the photo below to the right, on the left is the vestibular system and the right is the cochlea. The vestibular system can be separated into 2 distinct pieces. The semicircular canals, and the otolith organs. The otolith organs are your linear motion detectors, and the semicircular canals are your angular motion detectors. These two parts work together to help you know where you are in space, all the time! what an amazing system, to be able to work together always to figure out where you are in space!


What are vestibular disorders?
The vestibular system works very well overall. but, just like all other organs, things can go wrong. Generally, we classify things that go wrong with the vestibular system into two categories, central disorders and peripheral disorders. We will go further into each of these, but a vestibular disorder is what happens when some part of the vestibular system is injured or has an illness. The issue can come from many many different causes and triggers. For example, a vestibular neuritis can come from a viral infection, where vestibular migraine comes from a genetically linked migraine disorder. There is no one size fits all diagnosis or treatment of vestibular disorders. And, we need to remember it’s definitely possible to have more than one! Next, let’s dive into what central and peripheral disorders are more specifically.
What are central vestibular disorders?
A central vestibular disorder refers to a disorder of the brain and spinal cord. Specifically, these disorders do not occur in your actual vestibular system, rather in the central nervous system itself and how it processes vestibular input from your peripheral vestibular signals. Your vestibular system sends signals to your brain all day every day, constantly. It tells you where you’re looking and how fast your going, and so much more! When you have a central disorder, like vestibular migraine for example, the vestibular system itself is sending your brain the signal about where you are in space, but the brain is not receiving and translating the signal accurately. So, then you are in a mismatch between your internal signals, which causes symptoms like the feeling of being on a boat and general dizziness (and so much more!).
The most common central disorder is Vestibular Migraine (by FAR!), but other common ones are concussion, and Persistent Postural Perceptual Dizziness (PPPD). These disorders are common in the world of vestibular disorders, but they’re not the only reasons for central dizziness.
What are peripheral vestibular disorders?
A peripheral vestibular disorders is a disorder of the vestibular system itself. The vestibular system, pictured above, is the part in your inner ear that tracks vestibular signals and sends them to your brain through your vestibulocochlear nerve. These kinds of disorders are ones such as vestibular neuritis, benign paroxysmal positional vertigo (BPPV), acoustic neuroma, vestibular labyrinthitis, and Meniere’s Disease. These disorders are all so different from one another, but they all occur in the vestibular system itself.
This causes the wrong signal to be sent to the brain, which causes dizziness and vertigo, imbalance, difficulty walking in the dark, and more.
So, when your move your head or turn in a circle, or when you’re just walking around, your brain and vestibular system aren’t talking to each other correctly and dizziness occurs.
Can I have both central and peripheral vestibular disorders?
Central and Peripheral vestibular disorders can absolutely happen together at the same time. You can have many vestibular diagnoses together at one time, which can make them hard to parse apart. Almost all vestibular disorders have the same symptoms – dizziness, imbalance, rocking and swaying, vertigo, and others – but it’s important to remember that we need to differentiate between the two!
For example, you could have Vestibular Migraine, Meniere’s Disease, Benign Paroxysmal Positional Vertigo (BPPV), and Persistent Postural Perceptual Dizziness (PPPD). You may have room spinning vertigo from Meniere’s Disease, Vestibular Migraine, and BPPV, but you would not have room spinning from PPPD. Finding a doctor who is able to differentiate between each of these with you is incredibly important.
A vestibular informed provider will be able to distinguish between these diagnoses accurately. Typically a neuro-otologist and a vestibular physical therapist team is going to help you be able to determine which one (or multiple) are affecting you and your body!
Will I be dizzy forever?
No. Dizziness does not have to be forever. Even if you have been dizzy for 20+ years, there is hope! In The Oak Method, which is Dr. Oak’s Method of managing Vestibular Disorders, we will figure out what’s going on for you specifically, and use the basics to help you manage the dizziness and get back on track with your life!
There are no cures, but there are ways to manage your dizziness such that you will NOT be dizzy forever!
Ask yourself: How do I support my body today?
In the fast-paced and demanding landscape of modern life, the importance of self-support cannot be overstated. As we navigate various responsibilities, stressors, and challenges, it becomes imperative to establish a daily routine centered around the question, “How can I support myself today?” This article explores the multifaceted aspects of self-support, offering a comprehensive guide on how to nourish your body, mind, and spirit each day. From mindful practices to nutritional choices, the journey of self-support is not just a daily ritual; it’s a commitment to holistic well-being.
Mindful practices for mental well-being
Daily reflection and intention setting
Begin your day with a moment of reflection. Ask yourself, “How can I support myself today?” This simple yet powerful question sets the tone for mindful living. Take a few minutes to center yourself, acknowledge your feelings, and set positive intentions for the day ahead. This practice cultivates self-awareness and helps you approach the day with a proactive and intentional mindset.
Incorporating mindfulness meditation
Mindfulness meditation is a transformative practice that supports mental well-being. Carve out time each day for mindfulness meditation, whether it’s a short guided session or a moment of focused breathing. This practice enhances self-awareness, reduces stress, and fosters a sense of inner calm. As you ask yourself, “How can I support myself today?” weaving mindfulness into your routine becomes a cornerstone of mental resilience. You may weave this into your general daily routine, or make it a specific meditative practice (We have quite a few of these in VGFit!
Journaling for emotional release
Emotional well-being is a crucial aspect of self-support. Consider maintaining a daily journal to express your thoughts, feelings, and gratitude. The act of journaling provides a healthy outlet for emotional release, allowing you to process experiences and gain insights into your emotional landscape. This practice aligns with the daily inquiry of self-support, encouraging a continuous dialogue with yourself.
Physical nourishment and support
Prioritizing nutrient-rich foods
Nutrition plays a pivotal role in supporting your body each day. As you ponder the question, “How can I support myself today?” consider the impact of your dietary choices. Prioritize nutrient-dense foods such as fruits, vegetables, whole grains, and lean proteins. These foods provide essential vitamins and minerals that contribute to overall well-being, energy levels, and immune function. If you are in the holiday challenge, comment that you read this article for 2 points!
Staying hydrated for optimal function
Hydration is often overlooked but is fundamental to supporting your body’s functions. Make a conscious effort to drink an adequate amount of water each day. Proper hydration aids digestion, improves cognitive function, and supports joint health. Asking yourself, “How can I support myself today?” includes recognizing the role of hydration in maintaining your body’s vitality. In fact, if you are dehydarted, and most people are, you can present dizzier and more imbalanced than someone who is hydrated.
Regular exercise for physical vitality
Physical activity is a cornerstone of self-support. Engage in regular exercise that aligns with your preferences and fitness level. Whether it’s a brisk walk, a yoga session, or a high-intensity workout, exercise contributes to cardiovascular health, enhances mood through the release of endorphins, and promotes overall physical vitality. Integrating movement into your daily routine is a powerful response to the question of self-support. If you feel like you can’t exercise because you’re dizzy, Vestibular Group Fit is here to help – totally safe workouts deigned for vestibular warriors every single weekday! Join us here.
Cultivating emotional resilience
Setting boundaries for emotional well-being
Establishing healthy boundaries is an integral part of supporting yourself emotionally. Reflect on your commitments and relationships, and be mindful of your limits. Saying ‘no’ when necessary is an act of self-care. By recognizing your emotional boundaries and communicating them effectively, you create a supportive environment that honors your emotional well-being.
Seeking social support and connection
Human connection is a fundamental aspect of emotional resilience. Foster meaningful relationships and seek support from friends, family, or a support network. Share your thoughts and feelings, and be receptive to the support offered by others. By building and maintaining social connections, you create a strong emotional foundation that bolsters your ability to navigate life’s challenges.
Practicing self-compassion
Self-compassion is the art of treating yourself with kindness and understanding, especially in the face of difficulties. As you contemplate how to support yourself each day, integrate self-compassion into your mindset. Acknowledge your imperfections without judgment, and cultivate a compassionate inner dialogue. This practice enhances emotional resilience, fosters a positive self-image, and contributes to overall well-being.
Balancing work and rest
Time management for productivity and relaxation
Balancing work and rest is crucial for sustained well-being. Evaluate your daily schedule and prioritize tasks based on importance and urgency. Allocate dedicated time for work, but also ensure you schedule periods for relaxation and leisure. Striking a balance between productivity and downtime is an essential aspect of self-support. Practice saying no in the mirror (yes, really!!), it will help over time.
Quality sleep as a pillar of well-being
Quality sleep is a non-negotiable component of daily self-support. Prioritize a consistent sleep schedule and create a sleep-friendly environment. The rejuvenating effects of adequate sleep extend beyond physical health; they positively impact cognitive function, mood regulation, and overall resilience to stress. Answering the question of self-support involves recognizing the profound importance of restorative sleep
Mindful rest and recreation
In addition to sleep, incorporate mindful rest and recreation into your daily routine. Engage in activities that bring joy, relaxation, and fulfillment. Whether it’s reading a book, practicing a hobby, or spending time in nature, these moments of intentional leisure contribute to a well-rounded approach to self-support.
Supporting yourself each day is a dynamic and holistic endeavor that encompasses mental, emotional, and physical well-being. By consistently asking, “How can I support myself today?” and implementing the practices outlined in this guide, you embark on a journey of self-nurturing that transcends daily routine—it becomes a philosophy of intentional living. As you weave mindfulness, nutrition, movement, emotional resilience, and rest into your daily life, the cumulative effect is a flourishing sense of well-being that empowers you to navigate life’s challenges with grace and vitality.
If this is something you’re interested in getting more help with, Vestibular Group Fit is here to help!
Why we should practice daily gratitude for dizziness
In the hustle and bustle of our daily lives, it’s easy to get caught up in the chaos and lose sight of the positive aspects that surround us, especially when we are managing a chronic illness like a vestibular disorder. Amidst the challenges, stressors, and uncertainties, practicing daily gratitude emerges as a powerful tool to foster a mindset of appreciation and unlock a cascade of benefits for our mental, emotional, and physical well-being. Additionally, recent studies have suggested that incorporating gratitude into daily life may offer unique advantages for individuals dealing with chronic illness and dizziness, making this practice even more compelling for those facing health challenges.
The neuroscience of gratitude
Rewiring the brain for positivity
Research in neuroscience has shown that the brain is malleable, and its structure can be influenced by our thoughts and behaviors. When we engage in a daily gratitude practice, we are essentially rewiring our brains to focus on the positive aspects of life. This not only promotes emotional well-being but may also have implications for individuals dealing with chronic illness, where maintaining a positive mindset can contribute to overall coping strategies and improved quality of life. Additionally, for those experiencing dizziness, the positive neural changes induced by gratitude may play a role in stabilizing the emotional response to physical symptoms, and reduce the number of physical symptoms we may experience.
The role of neurotransmitters in gratitude
Gratitude has been linked to the release of neurotransmitters such as dopamine and serotonin, commonly associated with feelings of pleasure and happiness. For individuals with chronic illness, the neurochemical impact of gratitude may offer a natural and accessible way to elevate mood and potentially alleviate symptoms of anxiety or depression. Similarly, for those grappling with chronic dizziness, the release of these neurotransmitters could contribute to a an easier shift in emotions from negative to neutral or positive, which may positively influence the perception and experience of dizziness.
Gratitude and the stress response
Chronic stress is a pervasive challenge in modern society, and its detrimental effects on health are well-documented. Engaging in a daily gratitude practice has been found to modulate the body’s stress response. For individuals with chronic illness, managing stress is often a crucial component of their overall well-being, and the stress-reducing effects of gratitude can be particularly beneficial. Additionally, for those experiencing dizziness, which can be exacerbated by stress, gratitude may act as a protective factor, helping to mitigate the impact of stress on both mental and physical health – as well as chronic dizzy symptoms themselves.
Cultivating emotional resilience through gratitude
Shifting perspectives in adversity
Life is filled with ups and downs, and our ability to navigate challenges depends, in part, on our mindset. Gratitude acts as a powerful tool for shifting perspectives, especially in the face of adversity. For individuals dealing with chronic illness, the ability to find moments of gratitude can provide a sense of control and agency, fostering emotional resilience in the midst of health-related challenges. Similarly, for those experiencing dizziness, cultivating a positive perspective through a regular gratitude practice may contribute to a solid emotional foundation in the face of physical symptoms, which makes resilience in light of an attack easier. No, it’s never ‘easy’ but we do want to build a toolkit of ways to make it easier overall. Gratitude practices help!
Fostering connection and social support
Gratitude is not always an individual practice; it has the remarkable ability to strengthen social bonds and foster a sense of community. For individuals with chronic illness, the support of friends and family is often integral to their journey. Expressing gratitude within these relationships can deepen connections and provide a robust social support system. Likewise, for those dealing with dizziness, a supportive social environment cultivated through gratitude may serve as a crucial pillar in managing the emotional and practical aspects of their condition. For example, working with your loved ones on how they can specifically help you during attacks, practicing gratitude when they help, and also helping others in your life while they are grateful for your help. This is a multidirectional relationship and help can be both given and received; and the practice of gratitude goes both ways.
Gratitude as a coping mechanism
In times of crisis or personal struggle, the practice of gratitude serves as a coping mechanism. For individuals with chronic illness, navigating the emotional toll of their condition requires adaptive coping strategies, and gratitude can provide a constructive and empowering outlet. Similarly, for those experiencing dizziness, integrating gratitude into their coping toolkit may be a part of a holistic approach to managing the emotional challenges associated with the unpredictability of their symptoms. Gratitude becomes a psychological anchor during challenging times, helping individuals with chronic illness and dizziness to weather the storms of their respective health journeys with greater resilience.
The holistic impact on well-being
Gratitude and physical health
The mind-body connection is a well-established concept, and the impact of gratitude extends beyond the realm of mental and emotional well-being. For individuals with chronic illness, maintaining physical health is often a delicate balance, and gratitude practices have been associated with improved immune function and better sleep quality. Similarly, for those experiencing dizziness, the potential positive impact on physical health through gratitude may contribute to an overall sense of well-being and gratitude for their own bodies. For example, on the days where you’re feeling better it’s often helpful to thank your body for what it did that day! After moving your body, or doing an activity, or just after a long day shifting from ‘I feel so tired, I can’t believe my body can’t do as much as it used to,’ to ‘I am grateful for what my body was able to do today’ can be very impactful.
Gratitude and personal growth
A daily gratitude practice is not merely a tool for maintaining the status quo; it serves as a catalyst for personal growth and self-improvement. For individuals with chronic illness, the journey is often marked by continuous learning and adaptation. Gratitude becomes a vehicle for embracing change, learning from experiences, and evolving into a stronger, more resilient self. For those dealing with dizziness, the practice of gratitude may encourage a growth-oriented mindset, empowering them to navigate the challenges of their condition with a sense of purpose and self-discovery.
Creating a gratitude ritual: practical tips for daily practice
To harness the transformative power of gratitude, it’s essential to establish a consistent and intentional daily practice. For individuals dealing with chronic illness and dizziness, the incorporation of gratitude into daily routines provides a structured approach to managing the emotional and physical aspects of their health journey. From keeping a gratitude journal to expressing appreciation in relationships, these actionable steps empower individuals to make gratitude an integral part of their lives, offering a practical and holistic approach to well-being. By demystifying the process and offering practical guidance, this section aims to inspire readers, including those facing health challenges, to embark on their own gratitude journey.
The practice of daily gratitude transcends a mere habit; it becomes a catalyst for profound transformation in our lives. From rewiring the neural pathways in our brains to fostering emotional resilience and contributing to holistic well-being, gratitude emerges as a powerful force that can positively impact every facet of our existence. As we navigate the complexities of modern life, cultivating a daily gratitude practice offers a simple yet potent tool for unlocking joy, resilience, and an enduring sense of fulfillment.
Did you make it to the end of this article? Comment on the Facebook Post your favorite tip for gratitude, or reason to practice gratitude, for 2 extra bonus points!

Living with vestibular disorders can be a challenging journey, filled with ups and downs that extend beyond the physical symptoms. For the vestibular warrior in your life, finding the right gifts that provide comfort, relief, and support can make a world of difference. In this article, we will explore eleven specific gift curated for individuals facing the daily battles of vestibular disorders. In a world with infinite options, use these to help you widdle the options down and get something special for the vestibular warrior in your life!
The Dizzy Box
by Ruhewell x The Vertigo Doctor
Jill from Ruhewell is alllllll about a holistic approach to relief – and so am I – that’s why we put together The Dizzy Box. Ruhewell takes a unique and holistic approach to alleviating the symptoms of migraine and headaches, no matter which phase of your attack you may be in! This all-natural product line, enriched with essential oils, is carefully curated to cater to each phase of an attack. From the onset to the aftermath, the Dizzy Boxy offers a comforting solution for vestibular warriors seeking relief. The Dizzy Box bundle was hand selected by me, Dr. Madison, PT, DPT, to cater to your vestibular specific needs! Even better is it comes boxed in a cute presentation, so that’s just one less thing you need to think about! Check it out here.
For the coffee lover in your life
Swiss Water Process Decaf Coffee and a ‘Make Mine Decaf’ Insulated Mug. For many vestibular warriors, caffeine can be a trigger for their symptoms. Enter the better world of SWP decaf – that’s decaf without the chemical taste. Grab a bag of Swisswater process decaf coffee and pair it with a ‘Make Mine Decaf’ mug designed by me, The Vertigo Doctor! This gift not only acknowledges their unique dietary needs but also adds a touch of warmth and coziness to their daily routine.
Avulux Glasses
Protect your favorite vestibular warrior from light sensitivity, which is an all too common and frustrating symptom! Avulux Glasses are designed to reduce the impact of light sensitivity, a common challenge for vestibular warriors – and, they’re the only ones backed by research! Dive into the science behind these specially crafted glasses and explore how they can provide relief during challenging moments. From indoor lighting to outdoor glare, Avulux Glasses offer a stylish and functional solution to help your loved one navigate the world more comfortably.
Even better – grab these as an early gift to make your loved one’s holiday season easier! They’ll be able to wear them shopping online and in person to make shopping for their loved ones even easier this year!
Use code VERTIGODOC at checkout for a discount (codes stack for holiday sales)!

Vestibular 101
Vestibular 101 is the great jumpstart on healing for a vestibular disorder. Whether you’re in a rut, or you’re completely new to your vestibular diagnosis this is a great course for you! This course is designed by Dr. Madison Oak, PT, DPT, Dr. Emily Kostelnik, PhD, and Alicia Wolf! The three of us discuss movement, mindset, food, finding the right doctors, and more! Sign up here!!
Through Cyber Monday, it’s only $85!!
The Allay Lamp
Using similar technology as Avulux glasses, the Allay lamp uses green soothing light to help with light sensitivity. It is a great way for anyone with migraine or vestibular migraine to wind down at the end of the night! The Allay Lamp is a light source specifically designed for individuals with light sensitivity to use during times or heightened symptoms, or before bed to calm down! Delve into the technology behind this unique lamp and understand how it can create soothing environments, promoting relaxation and ease. This gift goes beyond the ordinary, contributing to a home that nurtures well-being. Explore the Harvard founded science behind Allay here!

This Is My Healing Era Hoodie
This is 2023, and let’s be real here – everyone is trying their best to heal from one thing or another! Secretly, I think it’s safe to say most of us are in our healing era. Personally, I am, and when I finally got my hoodie, I’ve not taken it off since then! It’s wearable comfort and empowerment as a reminder to prioritize yourself daily, ultimately building clothing can be a source of comfort and self-expression. Explore the significance of the This cozy garment can provide physical comfort while also serving as a powerful statement of empowerment. Everyone has a healing era, I know I am in mine (Dr. Madison here!!), but your loved one might be, too! This sweatshirt is a great reminder of what’s to come when you slow down for speedier healing! Get it here!

Vestibular Group Fit
If you are a vestibular warrior, Vestibular Group Fit is for you! Vestibular Group Fit is designed to make your life with a vestibular disorder so much easier, and more straightforward. If you or your loved one is struggling with a vestibular disorder, VGF is for you! It’s simple, you register, take a quick quiz, and you’ll be directed to everything you specifically need to know to manage your vestibular disorder. That, paired with meditations, workouts safe for your vestibular disorder, the best vestibular support group (where there’s endless help & support), and so much more! Plus, unlimited access to Dr. Madison Oak. Use code HOLIDAY at checkout for a discount!
The Skinny Confidential Ice Roller & Headache hat
Give the gift of ice this season! This ice roller is my personal favorite because it stays so cold for so much longer than other ice rollers – without melting all over your face like an ice cube does – and yes, I’ve made that mistake too many times! It’s an investment for an ice roller, so it’s an awesome gift for yourself or someone else. I got one for myself, and I use it every single day! It makes me look like I’m never puffy, it calms down any face pressure or pain, and when I have a rough night of sleep, I look less like I am working through a chronic illness, even though I am!
This headache hat is the one I see most often being used. It’s stretchy so no matter your head size it’ll work and can be worn at different levels! It can be down covering your whole nose (with room to breathe!) or just up on your forehead. This is SO helpful and so relieving – use with ice roller for maximum effect!
Rooted Behavioral Health Mindset Coaching
From Dr. Emily Kostelnik, PhD’s team, we have mindset coaching! Mindset coaching for dizziness disorders is a tailored approach that focuses on reshaping cognitive patterns and emotional responses associated with the dizzy anxious dizzy cycle. This specialized coaching aims to break the anxiety cycle often intertwined with dizziness, fostering a positive mental framework. By addressing negative thought patterns and fears related to dizzy spells, individuals can develop resilience and coping mechanisms. Mindset coaching involves cultivating mindfulness, encouraging self-compassion, and promoting a proactive attitude towards managing symptoms. Through guided exercises, individuals learn to reframe their perceptions of dizziness, reducing the impact of anxiety on their overall well-being. The coaching process empowers individuals to regain a sense of control over their lives, fostering a mindset that promotes acceptance, adaptability, and a more relaxed response to dizziness, ultimately contributing to improved mental and emotional well-being. Available worldwide.
Weighted Blanket
If you live with a vestibular disorder, you may often feel like you’re floating. If you don’t have a vestibular disorder but you’ve got a loved one with a vestibular disorder I am here to tell you: weighted objects are friends for vestibular disorders. This is because it helps to increase proprioception, and decrease the sensation of feeling ‘off’, and brings comfort during an attack! Now, most weighted blankets are not very cute, if I do say so myself! This one is so cute, comes in tons of colors, and is cozier than the others!
Hugaroo Warm Neck Wrap
Neck pain can happen for a few reasons, but no matter the reason sometimes you just need a heat wrap! The Hugaroo Wrap is a fan favorite vestibular warriors. This is a comforting accessory designed to provide gentle support and relief. This neck wrap can help you to feel calmer and feel your muscles relax. You just simply pop it into the microwave, and then place it on your shoulder for a weighted, heated, experience in helping you or your loved one neck and upper back! It feels so good!
The Way Out by Alan Gordon
This quick read is great for anyone experiencing chronic symptoms. Whether it’s dizziness, pain, or something else this book can help by giving you the tools to rewire your brain through somatic tracking. I, Dr. Madison, have found this book incredibly helpful for all my patients who read it as they gain a new understanding of neuroplasticity and signals of safety!
Dr. Madison LOVES the audio version of this book!!