Hormone levels change throughout the lifespan. Anecdotally, many of those with vestibular conditions appear to develop these conditions around these times of large hormonal changes. Let’s break down some of these milestones and how they relate to vestibular conditions.
Here is a quick breakdown of different time periods through a person’s life
- Prepubescent: infancy through puberty. 1-15 years old
- Reproductive age: after puberty, approx 15-40 years old
- Perimenopause: “around menopause” time before menopause when inter-menstrual irregularities and changes begin.
- Menopause: 12 months after final menstruation has occurred (1)
Prepuberty and Puberty & your Vestibular Disorder
One study has shown that in prepubescent males and females, the prevalence of migraine is equal at 4% occurrence. After puberty when a shift in hormones takes place and females have higher levels of estrogen, males with higher levels of testosterone, there becomes a dramatic change in migraine prevalence. After puberty, female prevalence in migraine is 18% and males is 6% (this is migraines in general and not vestibular migraines specifically). Part of what contributes to this change between males and females is attributed to the difference in estrogen levels. (2)
Pregnancy & Your Vestibular System
Typically, pregnancy has protective benefits from vestibular symptoms and migraines. The first trimester of pregnancy can be variable- some have worsening of migraines or new migraine symptoms such as an aura. Some experience migraines for the first time ever in the first trimester. In the second and third trimester there are higher estrogen levels which acts as a protection from migraines and most women typically experience improved symptoms. (3)
Talking to your doctor about supplements during and after pregnancy is important to keep you and your baby safe. Ask about B2, B6, folate, B12, vitamin D, magnesium, CoQ10, ginger, L-tryptophan and peppermint oil. (4)
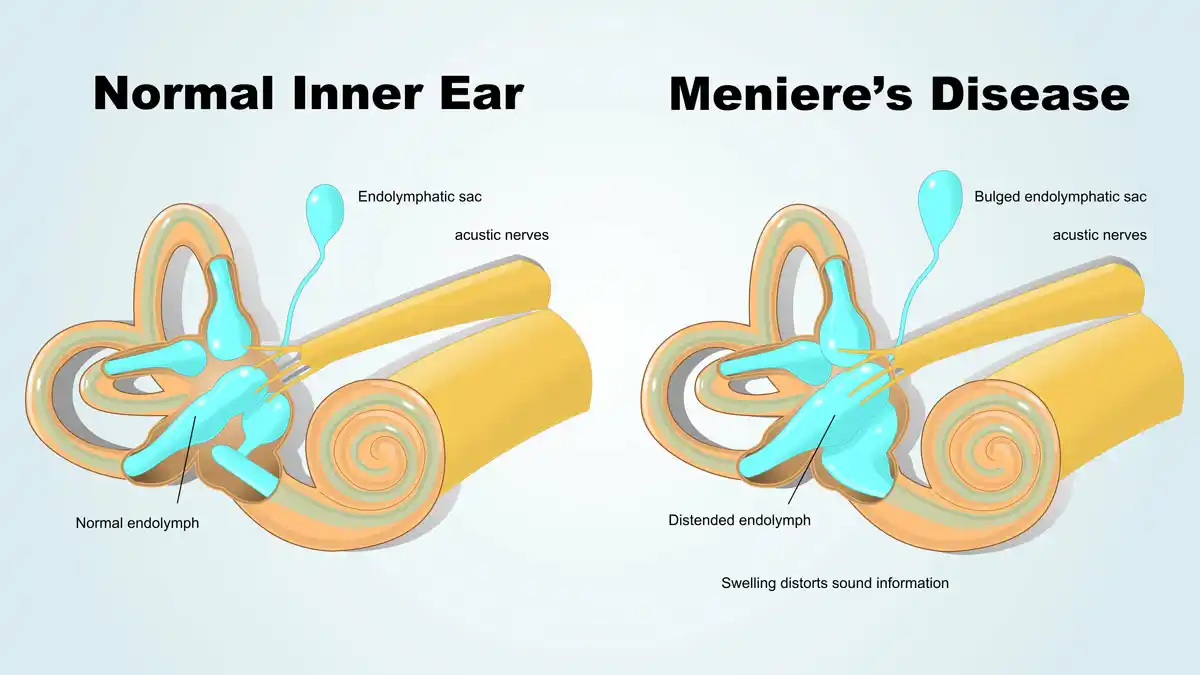
Meniere’s disease may have a worsening of symptoms in the first trimester from fluid retention and reduced particles in the blood. This can impact how fluid is distributed at the semicircular canals and cause an attack. A diuretic or low salt diet may be recommended by your doctor to assist with reducing attacks during the first trimester. (5)
Post Partum & Your Vestibular System
Immediately after giving birth, estrogen levels drop. This can result in exacerbation of migraine or vestibular migraine symptoms. Another hormone that can be involved is prolactin which helps with milk production after giving birth. Prolactin is controlled by the hypothalamus in the brain. There are theories that hypothalamus involvement is linked to migraines. Not everyone feels a worsening of migraines when breastfeeding, 50% feel that breastfeeding has been protective against migraines. (3)
Other factors to consider are postpartum depression and new stresses of being a parent of a newborn that can make you migraine or vestibular symptoms worse. Look above in the pregnancy section to see what supplements to ask your doctor about. (6)
Perimenopause & Your Vestibular System
Perimenopause tends to be the time where people are noticing new or changing vestibular symptoms or conditions. Those who never had a vestibular migraine before will start having VM (people with and without a previous migraine history). (7) Some theories around migraine believe that estrogens’ impact on serotonin (a neurotransmitter responsible for pain and mood) can create a cascade leading to a migraine. Estrogen impacts serotonin, serotonin impacts the trigeminal nerve, trigeminal nerve has CGRP which has been shown to be involved with migraine (7). Perimenopause is a time where estrogen levels are more erratic which results in periods becoming further or closer together (and less predictable). This can be one factor contributing to the onset or worsening of vestibular migraine in perimenopause. Perimenopause also has more vasomotor symptoms (hot/cold flashes for example) which can impact symptoms. Risk of depression also increases at this time. This can have a widespread impact in other areas of your life, but can also play into worsening symptoms (8).
Menopause & Your Vestibular System
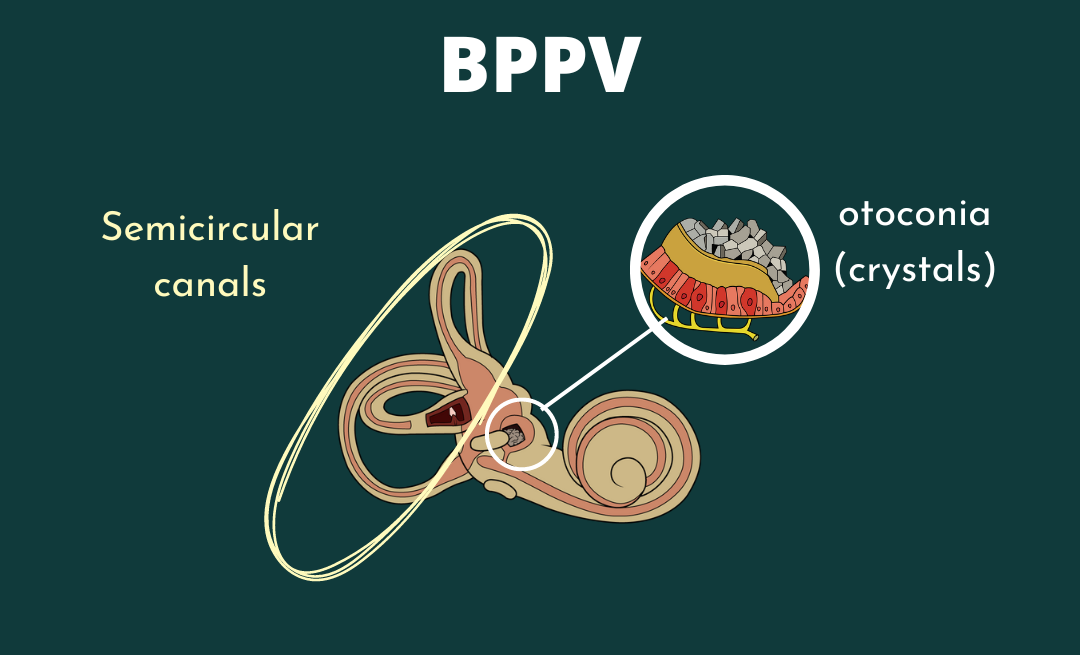
One full calendar year after one’s last period is considered menopause (1). Most with Meniere’s experience fewer attacks which can be theorized from fewer hormonal fluctuations (9). In this time of life, changes of BPPV increase and continue to increase as one ages. For migraines, there are fewer hormonal fluctuations but other contributing factors could continue to play a role in causing a migraine. It is important to continue to address these factors to optimize how you feel and gain control to manage your migraine (1).
Managing hormonal changes & Your Vestibular System
If HRT isn’t a great option for you, look at our previous article on Hormones and vestibular disorders to look at some other tips. Other things to keep in mind are:
- Address contributing factors (ex: neck or back pain)
- Exercise can assist with serotonin levels
- Certain foods can be helpful (think whole food/plant based food. Less processed foods)
Want to learn more about testosterone, oxytocin, progesterone and Q&A from other vestibular warriors?
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources:
- World Migraine Summit. (2022). How Women’s Hormones Affect Migraine. Retrieved April 2022.
- SD;, S. (n.d.). Sex hormones and headache. Revue neurologique. Retrieved April 21, 2022, from https://pubmed.ncbi.nlm.nih.gov/11139745/
- Sances G, Granella F, Nappi RE, Fignon A, Ghiotto N, Polatti F, Nappi G. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia. 2003 Apr;23(3):197-205. doi: 10.1046/j.1468-2982.2003.00480.x. PMID: 12662187.
- Beh, Shin C . Victory Over Vestibular Migraine: The ACTION Plan for Healing & Getting Your Life Back (p. 233). Beh Center for Vestibular & Migraine Disorders, PLLC. Kindle Edition.
- Andrews JC, Ator GA, Honrubia V. The Exacerbation of Symptoms in Meniere’s Disease During the Premenstrual Period. Arch Otolaryngol Head Neck Surg. 1992;118(1):74–78. doi:10.1001/archotol.1992.01880010078020
- Beh, Shin C . Victory Over Vestibular Migraine: The ACTION Plan for Healing & Getting Your Life Back (p. 229). Beh Center for Vestibular & Migraine Disorders, PLLC. Kindle Edition.
- Northrup, Christiane. (2015, May 29). Migraines. Christiane Northrup, M.D. Retrieved April 21, 2022, from https://www.drnorthrup.com/migraines/
- Migraine World summit. (2021). Overcoming Monthly Menstrual Migraine. Migraine World Summit. Retrieved 2022, from https://migraineworldsummit.com/talk/overcoming-monthly-menstrual-migraine/.
- NIH. (2016, April 25). Understanding how testosterone affects men. National Institutes of Health. Retrieved April 21, 2022, from https://www.nih.gov/newsevents/nih-research-matters/understanding-how-testosterone-affects-men