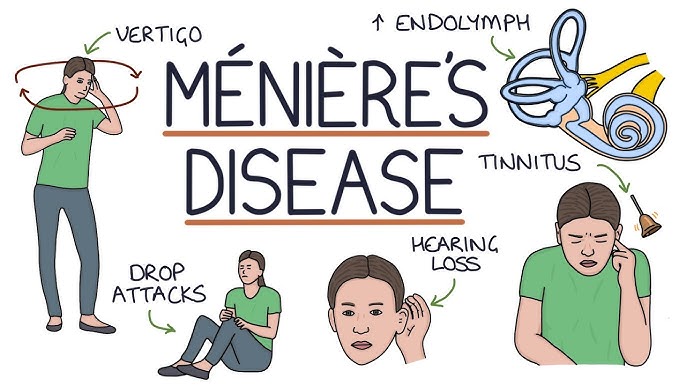
Living with Ménière’s disease—a chronic inner ear disorder characterized by episodes of vertigo, hearing loss, tinnitus, and a sensation of fullness in the ear—can be challenging. While there’s no known cure, various strategies can help manage symptoms and improve quality of life. These suggestions are here to help you better and more easily manage your life living with Meniere’s Disease, but are not the only options.
Ménière’s disease involves abnormal fluid buildup in the inner ear, leading to disruptions in balance and hearing signals. Symptoms can vary in frequency and intensity, making individualized management crucial.
Dietary and Lifestyle Modifications
1. Adopt a Low Sodium Diet/Possibly Low Histamine
Reducing salt intake to 1,000–1,500 mg per day can help decrease fluid retention in the inner ear, potentially minimizing vertigo episodes. This involves avoiding processed foods and being mindful of sodium content in meals. Many people also find that allergies spike due to histamine sensitivity so eating low histamine foods might also be helpful while living with Meniere’s Disease.
2. Limit Caffeine and Alcohol/Stop Smoking
Both substances can affect inner ear fluid dynamics and exacerbate symptoms. Limiting or avoiding coffee, tea, chocolate, and alcoholic beverages is often recommended. Smoking can also impact the inner ear, so avoiding smoking is also essential.
3. Stay Hydrated
Adequate hydration supports overall bodily functions and may help regulate inner ear fluid levels. Aim to drink sufficient water throughout the day. Try to get half of your body weight in ounces per day.

Medical Management:
4. Medications
Doctors may prescribe diuretics to reduce inner ear fluid pressure. During acute vertigo attacks, medications like meclizine or diazepam can alleviate dizziness and nausea. Diuretics that affect the vestibular system and inner ear tend to be helpful. Antihistamines can also help with neurotransmitters/hormones to improve inner ear circulation. It’s important to avoid medication that can cause fluid retention like NSAIDs.
5. Injections
For severe cases, intratympanic injections of steroids or gentamicin into the middle ear may be considered. While gentamicin can reduce vertigo, it carries a risk of hearing loss. Be sure to try other lifestyle modifications for Meniere’s Disease before going the injection route.
6. Surgical Options
This should be a last resort, but surgical options are available. The options are: Endolymphatic sac surgery, Labyrinthectomy, Vestibular Neurectomy, and Grommets AKA tympanostomy tube. While these options may help, there are many risks involved such as hearing loss, vision issues, paralysis in the face, and many more. For more information on these, you can join VGF.
Physical and Emotional Well-being:
6. Vestibular Rehabilitation Therapy
VRT involves exercises designed to improve balance and reduce dizziness by retraining the brain to compensate for inner ear dysfunction. Keep in mind that it is not for everyone! Starting with lifestyle modifications first is always recommended until symptoms are better under control.
7. Stress Management
Stress can trigger or worsen symptoms. Incorporating relaxation techniques such as yoga, meditation, or deep breathing exercises can be beneficial.
Practical Daily Tips:
8. Keep a symptom diary
Tracking symptoms can help identify potential triggers and assess the effectiveness of management strategies.
9. Use Supportive Devices
During episodes, using a cane or walker can provide stability. Some individuals find relief using acupressure wristbands or ginger products to alleviate nausea. Medications may also be prescribed to help with nausea.
10. Educate and Communicate
Informing family, friends, and coworkers about the condition can foster understanding and support. Joining support groups can also provide shared experiences and coping strategies. VGF is a whole community of people to support you on your journey!
Always remember that we have all the tools and resources you need to get better in Vestibular Group Fit. From dizziness management, to education specifically on Meniere’s Disease, we are here to help! To learn more and join, click here.