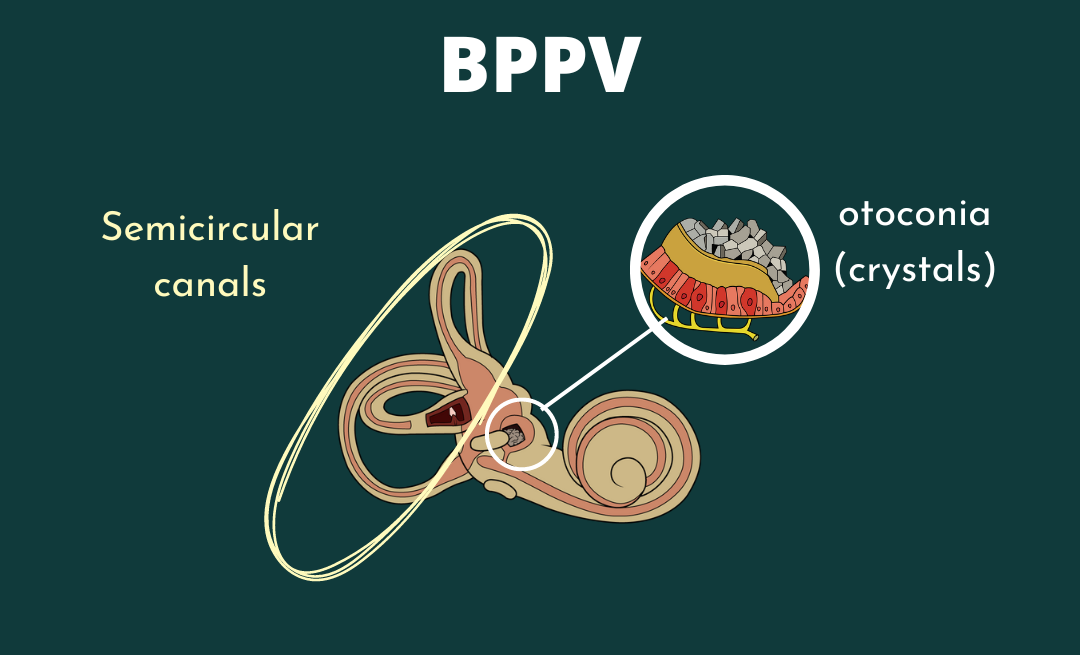
Ménière’s Disease is a chronic, frustrating, and incurable inner ear disease thought to be caused by a buildup of endolymph in the membranous labyrinth of your cochlea and vestibular system (1). This buildup of endolymph causes swelling on the membranous divide between the endolymph and perilymph, the Reissner’s membrane. This imbalance in your vestibular system causes symptoms of vertigo, spinning, hearing loss, and tinnitus. The potassium-rich endolymph flows into the perilymph, causing your symptoms until the membrane heals and the balance is restored (2). Ménière’s Disease is also commonly called Primary Endolymphatic Hydrops. It is different from Secondary Endolymphatic Hydrops as it has a rupture of the Reissner’s membrane and causes intermittent and/or sustained hearing loss. Because the hypothesis of the Reissner’s membrane rupturing is solely theoretical, there is a lot of room for research and rethinking the potential mechanism for Ménière’s Disease. However, regardless of the theory, we can treat your symptoms with a good healthcare team.
Symptoms & Diagnosis
Ménière’s Disease is associated with many signs and symptoms. It is important to recognize when they occur and differentiate between Ménière’s Disease and other causes of dizziness. The most common symptoms of Ménière’s Disease are: (1)
- Spontaneous, violent vertigo
- Fluctuating hearing loss
- Tinnitus and/or fluctuating hearing loss
The above symptoms occur regularly with Ménière’s Disease, but there are other ways to present as well. The following are less common, but can be frequent: (1)
- Anxiety
- Diarrhea, nausea, vomiting
- Cold sweats
- Heart racing/palpitations
- Blurry vision
- Eye jerking and/or nystagmus, feels like the room is spinning
- Trembling
Some patients know when an attack is about to happen. These symptoms almost mimic pre-migraine symptoms, however this is not a migraine. These include:(1)
- An “aura”
- Decrease balance
- Headache
- Increased inner ear pressure
- Tinnitus
- Hearing loss or sensitivity to sound, usually on one side
- Feeling of uneasiness
Knowing what your pre-Ménière’s symptoms are can help you move to a safer more comfortable space before the vertigo sets in. When you have a Ménière’s attack, try to keep tabs on these as a mental or physical list to be helpful to yourself.
Typically between Ménière’s attacks are asymptomatic, but for some there are symptoms that are lasting or sometimes occur between attacks. These kinds of symptoms tend to vary from person to person. Examples of symptoms are:(1)
- Difficulty concentrating
- Dizziness and/or lightheadedness
- Fatigue or sleepiness
- Sound sensitivity
- Hearing loss on one side
- Vision difficulties (blurriness, decreased depth perception)
- Unsteadiness (imbalance, falling, general stumbling)
The diagnosis of Ménière’s Disease can be complicated as symptoms come and go seemingly at random. There are specific diagnostic criteria in order to diagnose Ménière’s Disease. The following must be met in order to receive a diagnosis: (3)
- Two or more episodes of dizziness lasting from 20 minutes to 12 hours
- Audiometrically measured low- to medium- frequency sensorineural hearing loss in one ear defining the affected ear on at least one occasion before, during or after one of the episodes of vertigo
- Fluctuating aural (ear) symptoms such as tinnitus, hearing loss, fullness, in the affected ear
- Not better accounted for or diagnosed as another vestibular disorder
Clinical tests also address and can help diagnose Ménière’s Disease. These tests are:(4)
- ElectroCochleoGraphy: measures electrical responses in your cochlea
- Audiometry: a hearing test
- Electronystagmography: tests eye movement in response to your ear stimulation with warm water or cold air
The diagnosis of Ménière’s Disease is the first step ini direction to the beginning of your treatment. Although there is no treatment to cure Ménière’s Disease, treating your symptoms can be simple and effective.
Treatment
Treatment for Ménière’s Disease is all about symptom management and improvement of symptoms of dizziness and imbalance. Most of the time conservative care is effective to treat Ménière’s, and surgical intervention is unnecessary. These conservative treatments are most often provided by a physical therapist and your physician. These avenues are dietary considerations, medications, and Vestibular Rehabilitation Therapy (VRT).
The first step in treatment is the reduction of sodium in a person’s diet. Dietary restriction can be more strict than just reducing sodium, however sodium is usually the best place to start. Other dietary considerations include dairy, gluten, alcohol, and other common allergens and digestive irritants. Adhering to these new dietary restrictions is important in treatment as it will help reduce the risk of Ménière’s attacks recurring more frequently by reducing your overall inner ear pressure fluctuation risk. If this alone is ineffective for you, your physician may prescribe physical therapy and/or medications to help abate your symptoms and control your fluids.
The two most common medications in Ménière’s Disease are betahistine and diuretics. Betahistine is a vestibular suppressant used by those with Ménière’s Disease to suppress the vestibular system without interfering with vestibular habituation or compensation; this is different from Meclizine which both suppresses the vestibular system and interferes with compensation (5). Physical therapy is very effective in treating the vestibular system through CRT. It assists in compensation and habituation, and can treat imbalance; read more about PT below.
The non-conservative options are much less common and are a last resort for those who have frequent and recurring Ménière’s Disease episodes. The first option is an intratympanic gentamicin shot. This injection destroys some vestibular tissue in one ear, therefore decreasing or eliminating the change of a vertiginous episode. There is a risk of significant hearing loss with this option, so be sure to try and consider other things first (6). The other option is a surgical procedure to reduce pressure in the inner ear; this is done very infrequently and is often ineffective.
There are numerous treatments for Ménière’s Disease. Beginning with conservative treatments and working toward more intensive, invasive options is typically what I see in my patients. However, choosing with your healthcare team what is right for you is always the best option.
Physical Therapy
The goal of physical therapy in vestibular disorders is to treat symptoms of imbalance and lightheadedness, especially in those with Ménière’s Disease between attacks. After an episode, it is common for you to be tired, and laying down to recuperate for some time is normal and expected. However, when you begin to feel better it is important that you begin to move around to move your head when you’re feeling better. You just had an attack on your vestibular system, which now is unbalanced and is looking for input to help re-weight itself. By moving your head, you are assisting your vestibular system process and accommodate changing signals. Too much too soon can also be difficult, and you may want help grading your exercises. A physical therapist is the choice of a provider for help, he or she will be able to find exercises that help you rehabilitate your vestibular system in a way that will slowly improve your tolerance to activity and increase your balance. Often, your vestibular system will cause feelings of lightheadedness and nausea, and this can mean we’ve dont too much or not enough. Finding the fine line between the two is vital for a solid treatment plan.
Other Safety Considerations
When balance and mobility problems pop up, trips, and falls are more likely to occur. But many folks don’t realize the full spectrum of potential household hazards that can increase the likelihood of a stumble. With that in mind, NCOA created this guide, Home Safety for Older Adults: A Comprehensive Guide.This actionable PDF checklist that readers can use to ensure they or their loved ones remain safe at home.
This piece includes a wide variety of practical tips and recommendations from senior safety experts, including:
- Seasonal and material considerations for exterior home safety
- Suggestions for accessibility of everyday items
- Products to help older adults age in place safely
Sources:
(1) VEDA. (2020, June 24). Ménière’s Disease. Retrieved September 01, 2020, from https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/menieres-disease/
(2) Gibson, W. P. (2017, August 31). Revisiting the Cause of the Attacks of Vertigo During Meniere’s Disease. Retrieved August 30, 2020, from https://www.jscimedcentral.com/Otolaryngology/otolaryngology-4-1186.pdf
(3) Lopez-Escameza, J. A., Carey, J., Chung, W., Goebeld, J. A., Magnusson, M., & Mandalàf, M. (2015, February 10). Diagnostic criteria for Menière’s disease. Retrieved August 30, 2020, from https://content.iospress.com/download/journal-of-vestibular-research/ves00549?id=journal-of-vestibular-research/ves00549
(4) Martel, J. (2013, January 27). Meniere’s Disease: Symptoms, Causes, Treatments, and More. Retrieved September 01, 2020, from https://www.healthline.com/health/menieres-disease
(5) Lacour, M., Van de Heyning, P., Novotny, M., & Tighilet, B. (2007, August). Betahistine in the treatment of Ménière’s disease. Retrieved September 01, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2655085/
(6) NIDCD. (2020, July 15). Ménière’s Disease. Retrieved September 01, 2020, from https://www.nidcd.nih.gov/health/menieres-disease