Visual Vestibular Integration: Why do busy environments make me dizzy?
Our body uses three main systems to know where we are in space and what needs to be done to be balanced and safe. Today’s focus is going to be on our eyes and inner ear working together with visual vestibular integration. Let’s talk about what this is, what happens when visual vestibular integration isn’t working, and what to do about it!
If you need a refresher on our body’s main systems for balance, click here to review our What is Balance article before reading on.
What is visual vestibular integration?
Visual vestibular integration is combining the information from our eyes and inner ear to carry out tasks to help with our balance. These two systems work closely together to help keep our vision steady when moving our body, head, or both at the same time. This is known as the vestibulo-ocular reflex (VOR).
The brain also uses visual and vestibular information to gather as much information about your environment and compares all this information to get as clear a picture as possible. This creates checks and balances to ensure that our brain knows what is going on and can respond correctly.
A good example of this is when you’re sitting in a parked car. The car next to you starts to back up, and you feel like you’re moving briefly. This is your eyes picking up the car backing up next to you and saying “hey we’re moving what are we going to do about it”. You quickly realize that you aren’t moving because your vestibular system kicks in and says “actually we aren’t moving, the eyes are seeing that other car move, we are SAFE”.
If you read the previous article What is Balance, you know there’s the proprioceptive system. We do use our proprioceptive system to compare sensory information with our eyes and inner ear- especially on uneven surfaces and to make sure any body movements are accurate and correct. This relationship is not the main focus of this article but it does exist! We’re focusing on the connection between the inner ear and eyes because of certain symptoms people experience when visual vestibular integration isn’t accurate, so keep reading on to learn more.
What happens if visual vestibular integration doesn’t work?
If the signal from our vestibular system isn’t sending or perceiving the correct information (BPPV, neuritis, VM etc), our brain starts to ignore what our vestibular system is saying and rely more on our visual system. Using only our eyes can result in busy environments making you feel dizzy or like you are moving when you really aren’t. The vestibular system isn’t being used in these situations to double check the information for our eyes. Things like busy areas like malls or restaurants, action scenes in movies, or first person video games can make your symptoms worse. Luckily, there are ways to work on reducing the reliance on your eyes and start using accurate vestibular information to feel better in busy environments.
How to promote visual vestibular integration.
Balance exercises that challenge vision help promote your vestibular and proprioceptive systems. With practice and gradual progression of these exercises, our brain starts to relearn how to listen to all 3 senses equally again. Consulting a trained and licensed vestibular therapist can help you safely progress these exercises and is strongly recommended. The goal is to start with sitting or standing balance exercises that make the visual and proprioceptive information hard to gather, so your brain has to rely on vestibular input to complete the exercise! This can be done in a variety of ways,a few ways a trained vestibular PT might accomplish this is:
- Eyes closed
- Eyes open with videos
- Firm surface
- Foam surface
- Standing feet apart or feet together.
There are many ways to tailor exercise individually and safely. Consult a professional to evaluate your specific needs and assist you in the safe progression based on your needs!
Want to learn more about visual vestibular integration, and other vestibular tools to get back to your daily life? Found out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
What is Persistent Postural Perceptual Dizziness (PPPD)?
In general, Persistent Postural Perceptual Dizziness (3PD or PPPD) is a condition resulting in long term dizziness that fluctuates in severity after an initial event or vestibular condition. Let’s break down the diagnostic criteria to better understand what 3PD and if this is something to seek out treatment for.
PPPD Diagnostic Criteria
Here’s the check list your provider is looking at to determine if 3PD is the correct diagnosis and to then proceed with the most up to date treatment for this condition.All five criteria must be met for a PPPD diagnosis so let’s take a look:
-
One or more symptoms of dizziness, unsteadiness, or non-spinning vertigo are present on most days for 3 months or more.
-
a. Symptoms last for prolonged (hours-long) periods of time, but may wax and wane in severity.
-
b. Symptoms need not be present continuously throughout the entire day
Translation: The dizziness does not have a spinning component and has lasted longer than 3 months. The dizziness or unsteadiness can vary in severity and get better or worse over hours or days, but is present a majority of the time.
-
Persistent symptoms occur without specific provocation, but are exacerbated by three factors:
-
a. Upright posture,
-
b. Active or passive motion without regard to direction or position, and
-
c. Exposure to moving visual stimuli or complex visual patterns.
Translation: Upright positions like sitting or standing feel worse than lying down. Both active motion (walking, bike, jogging) and passive motion (riding in a car or being pushed in a wheelchair) can both be aggravating no matter the position or direction you are in during the movement. And finally, busy environments or patterns can make symptoms worse (ex: busy crowds, walking by fences, changing sunlight from bright to shadows).
-
The disorder is precipitated by conditions that cause vertigo, unsteadiness, dizziness, or problems with balance including acute, episodic, or chronic vestibular syndromes, other neurologic or medical illnesses, or psychological distress.
-
a. When the precipitant is an acute or episodic condition, symptoms settle into the pattern of criterion 1 as the precipitant resolves, but they may occur intermittently at first, and then consolidate into a persistent course.
-
b. When the precipitant is a chronic syndrome, symptoms may develop slowly at first and worsen gradually.
-
Symptoms cause significant distress or functional impairment.
-
Symptoms are not better accounted for by another disease or disorder. 1
Can You Treat PPPD?
Yes yes yes!Personally, we have found high PPPD treatment success when we stick to the four general steps to treating PPPD:
- Find the underlying cause
- Treat the anxiety
- Initiate Vestibular Rehabilitation Therapy
- Reduce safety behaviors (return back to daily life)
Want to Learn More About Treating PPPD?
If you’re interested in learning more about the specific factors address in VRT to reduce PPPD symptoms, reach out to a vestibular therapist or consider joining our vestibular community that includes dozens of premium content modules of information and resources and a great community to support you! Click here for the Free Treating PPPD Masterclass Disclaimer: Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here. Resources- Staab JP, Eckhardt-Henn A, Horii A, Jacob R, Strupp M, Brandt T, Bronstein A. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Bárány Society. J Vestib Res. 2017;27(4):191-208. doi: 10.3233/VES170622. PMID: 29036855; PMCID: PMC9249299.
- Probs t T, Dinkel A, SchmidMühlbauer G, Radz iej K, L imburg K, Pieh C, Lahmann C. Psychological di s tres s longitudinal ly mediates the effect of vertigo symptoms on vertigo-related handicap. J Psychosom Res . 2017 Feb;93:62- 68. doi : 10.1016/ j . jpsychores .2016.11.013. Epub 2016 Nov 30. PMID: 28107895.
- Chiarel la, Giuseppe & Petrolo, C. & Riccel l i , Roberta & Giofrè, L . & Ol ivadese, G. & Gioacchini , F .M. & Scarpa, Alfonso & Cas sandro, E ttore & Pas samonti , Luca. (2016) . Chronic subjective di z z ines s : Analys i s of underlying per sonal ity factor s . Journal of Ves tibular Research. 26. 403- 408. 10.3233/VES-160590.
Food is medicine – nutrition and vestibular migraine with Kelli Yates, RDN
Food and diet can impact how we feel, and can play an important factor when it comes to the management of certain vestibular conditions. Your doctor may recommend certain dietary guidelines based on your vestibular condition and other factors (medications, other health conditions etc).
For vestibular migraine, certain foods can provoke your symptoms or trigger a migraine depending on how “full” your migraine threshold is on a given day. (click here to learn more about threshold/bucket theory and some additional information on migraine diets). If you’re not sure where to start with changing your diet, a registered dietitian or nutritionist can be a great resource and guidance in exploring how food can be medicine.
Kelli Yates, RDN, LD, CLT is a private practice registered dietitian and specializes in migraine and gut health. She became interested in this area while pursuing her own answers to help manage her migraine beyond medication. Kelli has self guided programs, 1 on 1 help with her personally, and great information that she shares with us all on her instagram (@the.migraine.dietitian).
Kelli sat down with Dr. Madison to discuss how food can impact our health, especially those with migraines of all types.
Kelli notes how food can be medicine as both a preventative and active treatment. In general, food is best used as a long term preventative. For migraine, this long term management of symptoms with food involves learning what foods provoke symptoms or trigger a migraine and in what quantity. Some foods may need to be avoided altogether and others you may be able to enjoy in moderation, it really depends on the person. An elimination diet can help reduce common food triggers for migraine and then you reintroduce foods to determine if they affect you.
Food can sometimes have an immediate effect. Peppermint and ginger can help with acute nausea and initial symptoms. Food schedules can also have a more immediate change on how you feel. Regular meal times/not skipping meals, or healthy snacks throughout the day can be a small change that could impact how you feel.
Here are some tips Keilli shared with us regarding diet and migraine:
- Reintroduce foods one at a time. There are many ways to introduce foods and a dietitian is a great resource to help tailor reintroduction to you!
- Low histamine diets are a temporary solution. If a low histamine diet helps, further care is needed to get to the root cause.
- Do what works best for you. Listen to your body on what feels good or bad. You know your body best. Keep that in mind before trying something that is suggested you try or you were told worked for someone else.
If you want to hear more from Kelli, follower her on instagram @the.migraine.dietitian or go to her website https://kelliyatesnutrition.com/
Kelli talks more about reintroducing foods, why low histamine diets are only temporary solutions, probiotics, gut health testing and anxiety around food in her talk with Dr. Madison.
Do you want to learn how to manage your vestibular disorder holistically, through diet and more?
Click here to Manage your Vestibular Disorder Better
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Vestibular disorders, especially Vestibular Migraine, can cause neck pain and cervicogenic dizziness. However, thankfully, these are both manageable with vestibular physical therapy and cervical (neck) physical therapy. The neck is a complex group of muscles, bones, joints, and other soft tissues that can easily make you feel ‘off’ or out of place.
Luckily, that feeling does not have to last forever. Cervicogenic dizziness and other neck dysfunctions are very treatable. One of my favorite ways to manage cervical issues is stretching. Here are my twoi favorite stretches:
Pectoral stretch
Your pec muscles are located in the front of your chest. You have 2 on each side, the pec major, and the pec minor. The pec major is larger and lays on top of the pec minor. To stretch them both, you need to perform 2 different stretches for best results. In this video we see three stretches.The first two stretch the pec major, and the last stretches the pec minor. The further up the doorway you place your hands, the more you’ll get into the pec minor.

Trapezius stretch
If the back of your neck is bothering you, it can come from your chest, but another great stretch is a trapezius stretch, which will help stretch the back of your neck. The back of your neck is made up of quite a few muscles, but the biggest one, which tends to feel knotty, is the trapezius muscle. Here’s my favorite way to stretch the back of my neck. Watch the video, and if you want a second stretch for a similar movement, don’t twist your head!

What else can help neck pain?
Other than stretching, many things can help with neck pain. General exercise, improving your posture, and taking breaks from sitting.
General Exercise?
Exercise is good for us. Whether or not we’d like to admit it, we know that it’s something we should participate in regularly. There are a few exceptions, but it’s statistically unlikely that you’re in that group of people. If exercise makes you dizzy, or you’re worried that it could make you dizzy, Vestibular Group Fit is the answer to your issue. Vestibular Group Fit is the all-in-one, holistic solution to strengthening your vestibular system, helping you to move, and more! This helps you get rid of your neck pain through movement, and will help you prevent dizziness attacks in the future!
Improving your Posture
Your posture is just as important as your mom said it would be. If you ever thought that you may be having dizziness BECAUSE of your neck, your posture could be playing a roll. Your posture is in charge of where your head is – it’s all about your neck. If you neck is giving your brain a ‘bad’ signal about where your head is in space, it gets confused and send a dizziness signal. But, it can be treated with Cervical Physical Therapy and Vestibular Group Fit!
Taking Breaks from Sitting
Sitting for too long can be harmful to our posture, and if we remember from above, our posture can make us feel dizzy if it’s poor. In a world where we all work from home, it can be easy to get into the routine of sitting at your desk and not leaving until you finish work, except maybe a trip to the kitchen or two (I am guilty of this myself). Instead, it’s vital to take sitting breaks. Every 45-60 minutes stand up, walk to get a glass of water (yay, hydration!), grab a snack, or just take a lap around the house. It doesn’t matter what you do, but set a timer and make it happen! It will help your neck, back, and vestibular system!
Your vestibular system is a vitally important structure located in your inner ear. It is responsible for balance, equilibrium, spatial awareness, and more. It is connected to the cochlea and depends on fluid, nerves, and ear crystals (otoconia) for function. Vestibular hypofunction is a common dysfunction and means that your vestibular system is functioning ‘less’ than it should be (hypo=less). A unilateral vestibular hypofunction is more common than bilateral, and that’s why you find so much more information on it on Google.
Unilateral vestibular hypofunction means that one of your vestibular systems is working suboptimally. Bilateral vestibular hypofunction means both of your vestibular systems are working suboptimally. In rehabilitating a unilateral dysfunction, the opposite side can be used to help you compensate for the other side. However, with bilateral vestibular dysfunction, both sides have some sort of dysfunction, and cannot be used to compensate, adapt, and/or habituate.
What Causes Bilateral Vestibular Hypofunction?
Bilateral vestibular hypofunction can come from many pathologies. Those with vestibular migraine, bilateral Meniere’s disease, history of meningitis, CANVAS, superficial siderosis, and others can cause bilateral vestibular hypofunction. Regardless of the causation, once you have bilateral loss it’s important to understand what it is, how to manage it, and how to take care of the rest of your health.
Symptoms of Bilateral Vestibular Hypofunction
- imbalance
- dizziness
- instability
- disequilibrium
- oscillopsia/gaze instability
- visual vertigo
- brain fog
- fatigue
- other cognitive deficits
If the bilateral vestibular hypofunction is a result of another neurological disease, you may also be experiencing alternative symptoms secondary to the diagnosis.
Bilateral Vestibular Hypofunction Management
Managing bilateral vestibular hypofunction is about much more than medication, in fact, in the chronic phases of bilateral vestibular hypofunction it’s recommended not to use medication, but o use vestibular rehabilitation therapy and exercise to promote healing (1). In a randomized control trial, those who underwent vestibular rehabilitation treatment had significantly better outcomes in function and balance than those who had no treatment or only used medications. This is likely because the mediations typically prescribed are vestibular suppressants and anti-emetics. Vestibular suppressants will actually hinder your system’s function further, and anti-emetics are only to treat the symptoms so nausea and vomiting associated with vestibular dysfunction.
Managing bilateral vesitbular hypofunction requires strengthening your physical body, improving the use of your proprioception, maintaining eye health, and continuing your general health. You have three balance systems, and one (your vestibular system) is not functioning at 100%, but strengthening the other two (vision and proprioception) will help you maintain the best balance possible. Additionally, taking care of your physical health, preventing other morbidities like diabetes or cardiovascular dysfunction, and staying as fit as you are able will help you keep your balance and equilibrium as much as possible.
What is Compensatiton
With a permanent injury to any system, the body uses another system or external resource (like a cane) to make up for the loss of the damaged system. In a unilateral vestibular hypofunction, the adaptation of the brain and opposite vestibular system returns your equilibrium to a new normal by rewiring brain pathways (through neuroplasticity). With bilateral vestibular hypofunction, since we cannot use the opposite system to adapt and compensate, you may need to employ other tactics.
For bilateral vestibular hypofunction, external compensation tactics are frequently a good idea. I recommend the following:
- A cane or walker for uneven or difficult environments
- Flat shoes with good match support so you are able to feel the floor (avoid shoes with high platforms or a heel)
- Wear migraine classes if you are light-sensitive
- Wear earplugs if you are sound sensitive
Bilateral Vestibular Hypofunction Requires…
A lot of attention to yourself and your balance systems. I know that this is true for all vestibular dysfunctions, but especially for Bilateral Vestibular Hypofunction. What questions do you have about BVH I can help you answer? Comment below, or shoot me an email!
Vestibular Group Fit has Premium Content dedicated to understanding Bilateral Vestibular Hypofunction. Strengthening your legs and body is one of the best things you can do to improve function and feel less wobbly with Bilateral Vestibular Hypofunction.
Sources:
(1) Horak FB, Jones-Rycewicz C, Black FO, Shumway-Cook A. Effects of vestibular rehabilitation on dizziness and imbalance. Otolaryngol Head Neck Surg. 1992;106(2):175-180. PMID:1738550
Mal de Debarquement Syndrome, or MDDS, is the sensation that you are still in passive motion, even when you have stopped the passive motion. Imagine you were on a plane or a boat, and that you step off. You momentarily may have sea legs, you may feel imbalanced or like you are going to lose your balance. Maybe you feel like you’re internally still swaying to the rhythm of the ocean. This is normal, there’s nothing to be concerned about here, this is not Mal de Debarquement Syndrome.
Mal de Debarquement Syndrome is when you chronically feel you’re in chronic passive motion after you disembark from a long trip where passive motion is involved. Typically extended boat, plane, or car rides.
MDDS can be spontaneous, but this is not as common. When you have non-motion-triggered, or spontaneous, MDDS, it typically comes from a stressful event or a large hormonal change. In a study, they found approximately 44% of people had symptoms onset in perimenopause or menopause (1). It’s important to consider your life stage when the diagnosis is being made.
MDDS Symptoms
MDDS symptoms are very specific, but they can also mock symptoms of vestibular migraine. Some people with vestibular migraine also feel as though they have MDDS, but that is frequently an incorrect diagnosis. MDDS symptoms are constant feeling of imbalance, rocking or swaying, feeling like you’re walking on an uneven surface. These are similar to vestibular migraine symptoms. BUT, MDDS always gets better when you’re in passive motion. People with MDDS very rarely have motion sensitivity or get car sick. Typically, the best part of their day is when they’re driving, on a boat, train, or plane.
- Fatigue
- Cognitive slowing
- Chronic internal motion
- Hypersensitivity to physical stimuli
- Imbalance
If these symptoms are spontaneous, they can actually be caused by hormonal changes or stress. These symptoms, again, get better with passive motion. This is different than chronic subjective dizziness, which is often confused with MDDS because chronic subjective dizziness gets worse with motion, while MDDS is better when in motion. Be sure to consider this when you believe you may have MDDS.
MDDS Treatment
MDDS can be treated in two ways. The gold standard for MDDS treatment is the Dai Protocol (2). This protocol treats MDDS with optokinetic stripes and passive head motion. In short, the MDDS Treatment discovered by Dai plays stripes in >90% o your vision, and someone moves your head in a right, left, center passive motion at approximately 12 Beats Per Minute. The direction of the stripes is determined by the opposite of the direction you feel you are being pulled, or by where you end up on the Fukada Stepping Test. This is repeated for 1-8 minutes, 1-8 times a day, for 5 days with a 30-minute interval in between. inn 17/24 patients, there was an immediate 75% improvement in symptoms. And, when looking back at the study they found that there may not have been all people with true MDDS – some may have had an inaccurate diagnosis and was likely why they did not see immediate improvement.
Physical Therapy for MDDS Treatment treats only the functional deficits. It can be done before or after the Dai Protocol is attempted. And these functional deficits should be focused on especially if walking, balancing, or gaze stability is difficult for you. Vestibular Rehabilitation Therapy is not done to completely rid you of your MDDS symptoms or rocking and swaying, but instead to improve your ability to function throughout your life, even if you feel you’re rocking and swaying.
MDDS Diagnosis
The diagnostic criteria for an MDDS Diagnosis are now clear, and stated below (1).
- Clinical history of oscillating vertigo
- Temporary improvement with re-exposure to passive motion
- The symptoms began within 48-hours of disembarking a trip from chronic passive motion (boat trip, plane ride, long duration road trip)
Remember, you must feel BETTER in motion, not worse, to receive a diagnosis. If you are in passive motion and feel worse, you are more likely to have chronic subjective dizziness, PPPD, or another vestibular dysfunction.
How Long Does Mal de Debarquement Syndrome Last?
MDDS lasts for an indefinite amount of time, especially when untreated. It is considered chronic if the symptoms do not disappear for more than 6 months. For some people, MDDS can last for the rest of their lives, and for others, it disappears as quickly and spontaneously as it appeared, especially if it had a spontaneous onset. If your MDDS symptoms ever do decrease or go away, it’s recommended to avoid the original stimulus that brought it on as much as possible. I know that this is easier said than done, as you may have gotten MDDS by being in a car and you probably still need to drive. In this case, I do recommend driving and going about your activities, do not practice avoidant behaviors, but do try to get out of the car and walk around, taking frequent breaks, if you’re on a longer trip.
How Do I Know if my Symptoms are MDDS or Vestibular Migraine?
This can be tough, but there are a few ways that I know whether it’s VM or MDDS as a clinician. You should always be asking your doctor/healthcare team for their advice, but here are my best tips to help you out.
- Do you have a history of migraine, or does migraine run in your family?
- Are you light sensitive, sound sensitive, or movement sensitive?
- Do your symptoms get worse with movement or when you’re in the car?
- Do you have specific attacks where symptoms tend to increase?
- Do you have chronic internal rocking that began after long-duration passive motion (plane, train, boat, etc)?
- Do your symptoms get better when you get in the car and go for a drive?
- Do you resonate with the term land-sick?
If you answered yes to questions 1-4, Vestibular Migraine is more likely than MDDS. If questions 5-7 sound more like you, MDDS is more likely. Remember that this is not medical advice, and you should always consult your doctor!
Sources:
(1) Cha, Y., Cui, Y., & Baloh, R. (2018, May 7). Comprehensive Clinical Profile of Mal De Debarquement Syndrome. Retrieved August 29, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5950831/
(2) Dai M, Cohen B, Cho C, Shin S, Yakushin SB. Treatment of the Mal de Debarquement Syndrome: A 1-Year Follow-up. Front Neurol. 2017 May 5;8:175. doi: 10.3389/fneur.2017.00175. PMID: 28529496; PMCID: PMC5418223.
Magnesium is an incredibly important supplement in our bodies, especially if we have migraine. Many studies have found that taking daily magnesium can help reduce migraine attack frequency and intensity. Typically the dose is 400-500mg/day for prevention, and then more for an acute dose if you’re trying to stave off an attack.
Types of Magnesium for Migraine
Magnesium Oxide
Magnesium oxide is the most common form of magnesium found in most stores, and if you pick up most drug store magnesium, it will likely be oxide. This is an affordable option and it’s in Class A of supplements, meaning it’s safe during pregnancy.
Magnesium Glycinate
Magnesium glycinate is the slightly less common form of magnesium, however its still easily accessible and does not cause the stomach upset that oxide does!
Magnesium Threonate
AKA CogniMag is something that many in the Vestibular Migraine community swear by for grain fog! IT’s a slightly different make up of magnesium and helps with improving cognition.
Magnesium in Foods
Many common foods are high in magnesium, and if you’d rather just try to eat enough throughout your day, you are welcome to try. The most common foods with high magnesium are beans/legumes, nuts and seeds, fiber-rich whole grains, dairy products, and many leafy greens. Although it’s entirely possible to get enough magnesium in your diet this way, it’s unlikely enough for a person with vestibular migraine, as a person with VM is typically low in magnesium, even if they eat a well-rounded diet.
Magnesium Spray
Magnesium spray is a topical form of magnesium that can help get magnesium into your bloodstream, without ingesting it orally. Because so many people are sensitive to magnesium in their gastrointestinal system, it’s not always an option to take it orally, even if you want to. A great place to start, other than your diet, are topical options! 4 sprays of this, on your skin, provides 66mg of magnesium! Although it’s a ways to get up to 400, it’s an excellent place to start!
Magnesium Lotion
Magnesium lotion, similarly to spray, is another topical option for you. This way, you won’t have gastrointestinal upset, but will still be able to increase the amount of magnesium your bloodstream absorbs. Additionally, it is a great way to practice self-massage on your neck. Take some of this cream, dab it on your neck, and rub your neck and shoulders for a neck-pain-relieving massage.
Magnesium Bath Soak
Sometimes when you are having a high pain migraine day, there’s nothing better than a warm bath. Pop this magnesium bath and foot soak in a bath of warm water and relax!
Magnesium Roller
The last option for non-oral magnesium is a roller. You can roll this anywhere on your body, it can sometimes help with sleep when put on your temples, or head pain relief!
Dizziness, vertigo, and anxiety create a vicious cycle. The short answer is yes; vertigo can be caused by stress. However, typically dizziness is caused by stress, not true vertigo. Even if you do not consider yourself to be an anxious or stressed person, there is a high likelihood that you will experience stress and/or anxiety after getting vestibular symptoms. This is because of the close relationship between the stress and anxiety center and the vestibular system.
What is Vertigo?
Vertigo is the incorrect perception that you or the room around you is moving or spinning. This can be in the form of room-spinning vertigo, typically from Benign Paroxysmal Positional Vertigo, or BPPV, or from Meniere’s Disease or Vestibular Migraine. Vertigo is not all dizziness, however many of us incorrectly name our sensations vertigo even when they are ‘dizzy’ by definition. Dizziness accounts for: lightheadedness, heavy-headedness, bouncy, floaty, and other terminologies. It’s important to distinguish the two different sensations as it can help your doctor or other healthcare provider determine an accurate diagnosis. Stress can be a factor causing vertigo and dizziness alike.
What Regulates Anxiety and Dizziness?
The Limbic system is made up of the amygdala, hippocampus, and hypothalamus; it regulates emotion and processes memory (1). Additionally, it is responsible for fear & aggression, and joy & excitement. The limbic system is tightly bound to the vestibular system through many synapses, so when you begin to get dizzy, you may start to feel stressed or anxious simultaneously. Research has shown that when pigs are given a lesion in their vestibular systems, they immediately begin to produce the stress hormone cortisol (2). Additionally, in a study done on people, when caloric testing is performed (which makes you dizzy), levels of stress hormones increased significantly, and those who are prone to motion sickness had already-elevated stress hormone levels (2). Our brains are not structured to endure lengthy durations of trauma or stress, which causes the link between anxiety and dizziness.
Neurons that fire together, wire together. – Donald Hebb
We have many neurons firing in our brains and nervous system; this is how our body functions. Our brains are plastic – meaning that our brains can learn and change constantly, as much as we need them, to suit our current needs. I’m going to repeat it: neurons that fire together, wire together. This phrase was coined by neuropsychologist Donald Hebb and describes how neuronal pathways form through reinforcement. If you’ve ever tried to learn a new skill, whether it was driving, playing violin, typing, or doing schoolwork, you likely noticed that the more you did something, the better you became at your new skill. The same rule goes for anything. If you find you are feeling dizzy and then immediately becoming anxious, or stressful thoughts begin to enter your head, it can make the dizziness increase exponentially. Neurons that fire for dizziness and then immediately cause anxiety wire together. This creates the dizzy-anxious-dizzy cycle.
Donald Hebb goes further into talking about why we should practice gratitude, which I think is vital for those with vestibular disorders. Wiring dizzy sensations with gratitude, or other positive sensations, can actually decrease dizziness overall.
How to Break the Dizzy-Anxious-Dizzy Cycle?
Dizziness can absolutely be caused by stress and, as we discussed above, if a stressed or anxious neuron is fired, over and over, at the same time as a dizzy neuron, the two will wire together. Breaking the cycle can be difficult, especially if it’s rooted deep within your brain from years of repetition. The gold standard for dizziness related to anxiety is vestibular rehabilitation therapy, cognitive-behavioral or acceptance and commitment therapy, and medical care.
Vestibular Rehabilitation Therapy and Anxiety
After a vestibular diagnosis, you may feel like you never want to move again – the less you move, the less dizzy you feel, right? Unfortunately, that line of thinking is false and disproven. However, that also means you are able to move freely and as much as possible! If movement feels scary to you, like you might fall over, or trigger a dizzy episode, vestibular rehabilitation therapy is right for you! Vestibular rehabilitation therapy provides a safe environment to help you return to movement without triggering severe symptoms. Being able to move with a vestibular physical therapist to perform functional movements shows your brain that you are safe, secure, and calm. This will remind your brain that moving does not have to make you feel dizzy, and regardless of your diagnosis, it will slowly recalibrate your brain to receive vestibular inputs correctly
If you have specific questions about Vestibular rehabilitation therapy, click here for more information.
Psychological Therapy and Anxiety
We think about going to therapy for typical stress, depression, and anxiety. However, we don’t consider going to therapy for vestibular needs nearly enough. Acceptance and Commitment Therapy (ACT) and Cognitive Behavioral Therapy (CBT) are both excellent kinds of therapy that work to decrease dizziness and improve function. Research shows that patients with chronic dizziness, especially PPPD, make improvements with therapy, especially when combined with vestibular rehabilitation therapy (3). Although there is not a randomized control trial at this time, the pilot study showed great results.
My favorite resource for all things dizziness-related therapy is Dr. Emily Kolstenik. She has two courses, Breaking the Dizzy-Anxious-Dizzy cycle, and Committing to Balance. One is a mini-version of the other, and they are both excellent resources for you if you’re looking to learn more about the vestibular system, decrease anxiety, improve your self-awareness in a healthy way, and decrease your dizziness symptoms.
Got to the end of this article? Comment that you read today’s article on the Facebook Group to get 2 extra Holiday Challenge points!
Sources:
(1) Gamba P. Vestibular-limbic relationships: Brain mapping. Insights Depress Anxiety. 2018; 2: 007-013. DOI: 10.29328/journal.ida.1001006
(2) Saman, Y., Bamiou, D., Gleeson, M., & Dutia, M. B. (1AD, January 1). Interactions between stress and vestibular compensation – A Review. Frontiers in Neurology. Retrieved October 5, 2021, from https://www.frontiersin.org/articles/10.3389/fneur.2012.00116/full#h3.
(3) Kuwabara, J., Kondo, M., Kabaya, K., Watanabe, W., Shiraishi, N., Sakai, M., Toshishige, Y., Ino, K., Nakayama, M., Iwasaki, S., & Akechi, T (2020, June 11). Acceptance and commitment therapy combined with vestibular rehabilitation for persistent postural-perceptual dizziness: A pilot study. Science Direct. Retrieved October 5, 2021, from https://www.sciencedirect.com/science/article/abs/pii/S0196070920303033?via%3Dihub.
Vestibular Migraine, as I’m sure you know by now, can be incredibly challenging to manage. Between weather changes, hormone changes, food triggers, and decreasing your caffeine intake, ‘a challenge’ doesn’t even begin to describe it. There’s a new study that I wanted to bring your attention towards, Dietary alteration of n-3 and n-6 fatty acids for headache reduction in adults with migraine: randomized controlled trial.
This article is interesting because instead of taking another thing out of your diet, it talks about something you can and should eat more of – finally!
What Food Group is Great for Vestibular Migraine?
This new study from the British Medical Journal shows that increasing Omega-3 Fatty acids, and without decreasing Omega-6’s can help decrease migraine pain, days, attacks, and other migraine-related symptoms.
The research shows that altering Omega-63s without changing Omega-6’s can decrease pain severity and frequency of attacks. However, the research did not find that there was a significant difference in quality of life.
What’s the Science between Omega-3’s and (Vestibular) Migraine?
Vestibular Migraine occurs due to a complex cascade of events that begins in the brain stem and trigeminal nerve, impacts the trigeminocervical complex, and then impacts the vestibular system. This cascade of events is what causes both pain (trigeminal nerve) and dizziness (vestibular nerve) in those with vestibular migraine. Omega-3’s are protective against that response.
As human beings, we are great at many things, however, synthesizing our own Omega-3 and 6’s is not one of them. Therefore, we can alter the number of fatty acids we have at any given time with our diet and/or supplements. And, it just so happens that these fatty acids are essential to the migraine cascade – in fact, they have a big role in pain regulation.
The nerve endings of the trigeminal nerve (the one that causes pain in migraine) are regulated by these same fatty acids, called lipid mediators. These mediators and together known as oxylipin receptors, and they’re enriched at the end of the trigeminal nerves. They regular sensitization and the release of the headache-related neuropeptide calcitonin gene-related peptide (1). This fact implies that there is a link between omega-6 & 3 fatty acids and headache etiology.
The oxylipins that come from Omega-6’s have been found to “sensitize the trigeminal nerve endings, and evoke behavioral pain responses;” this means Omega-6’s can increase pain severity and migraine frequency (1). However, the oxylipins that are derived from Omega-3’s are found to have antinociceptive properties, meaning that they reduce pain (1).
Where do I Find Omega-6’s, and Should they be Avoided?
Omega-6, the kind of fatty acid that is found mostly in the typical American diet, in fact, there is research to show that most people who eat a Western diet eat significantly more Omega-6s than Omega-3’s. Omega-6’s do play a role in our body’s function, so you should not completely get rid of this kind of fat. However, because we eat so much Omega-6, and want to try to fit in more Omega-3, it’s important to know where they come from.
- Vegetable oils
- Soybeans
- Corn/corn oil
- Eggs
- Some meat and fish
Where Do I Find Omega-3’s?
Omega 3’s are to kind of fatty acids we don’t get enough of in the Standard American Diet. It’si’mportant we get more of these than Omega-6’s so we can desensitize the trigeminal nerve, decrease pain severity, and decrease pain days overall. Although it may be easier for you to take them as a supplement, it is better to get them in your food, and more affordable. However, if you do not like any of these foods, it is typically recommended to get them in supplement form (aka Fish oil). Ask your doctor before you change or start a new supplement.
- Salmon, mackerel, or other fatty fish
- Seaweed and algae
- Chia and hemp seeds
- Walnuts
- Edamame
- Oysters & shrimp
- Spinach & Brussels
- Supplements
Source:
Ramsden, C. E., Zamora, D., Faurot, K. R., MacIntosh, B., Horowitz, M., Keyes, G. S., Yuan, Z.-X., Miller, V., Lynch, C., Honvoh, G., Park, J., Levy, R., Domenichiello, A. F., Johnston, A., Majchrzak-Hong, S., Hibbeln, J. R., Barrow, D. A., Loewke, J., Davis, J. M., … Mann, J. D. (2021, July 1). Dietary alteration of N-3 and N-6 fatty acids for headache reduction in adults with migraine: Randomized controlled trial. The BMJ. Retrieved October 5, 2021, from https://www.bmj.com/content/374/bmj.n1448.
Although there is a distinct difference between these two inner ear conditions, one can play a role in the other occurring. Benign Paroxysmal Positional Vertigo or BPPV is a type of true, room-spinning, vertigo caused by the displacement of otoconia from your otolith organs within your inner ear. Endolymphatic Hydrops, both Primary and Secondary, is related to a pressure-volume issue in the membranous part of your inner ear, which causes dizziness, sometimes vertigo, ear fullness, hearing loss, and more.
Before we get into the relationship between the two conditions, let’s understand what’s happening in each diagnosis.
Benign Paroxysmal Positional Vertigo
BPPV is the most common form of vertigo, and most of the time we have no idea why it happens. Tiny ear crystals, otoconia, fall out of the space they belong and into the semicircular canals, most commonly the posterior canal. When this happens, the otoconia sliding through the canals when you move your head causes nystagmus, or involuntary eye movement. This nystagmus then makes it look like the room is spinning. If you’d like more info on BPPV and nystagmus, click here.
Primary and Secondary Endolymphatic Hydrops
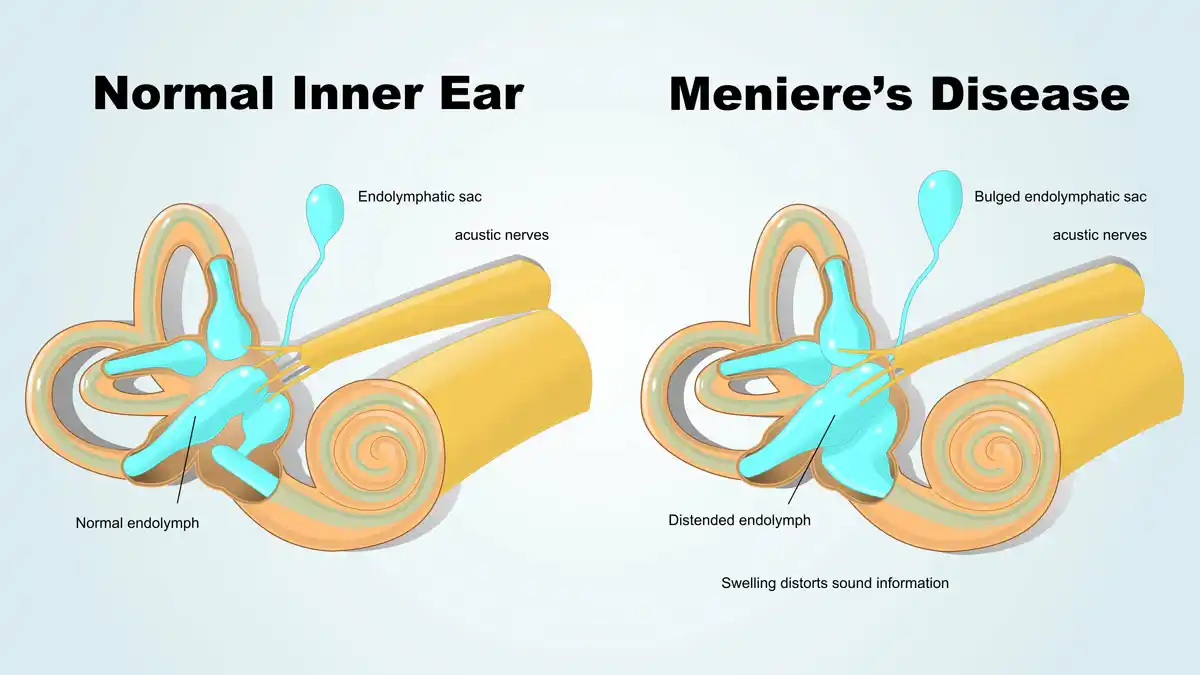
Primary Endolymphatic Hydrops, AKA Meniere’s Disease, and Secondary Endolymphatic Hydrops are a result of an inner-ear pressure-volume relationship dysfunction. Endolymph is the fluid within your ear canal, it is high in sodium, and water osmoses between the endolymph and the perilymph on the other side. When there is too much fluid, because of the laws of physics, more fluid goes toward the endolymphatic portion of the inner ear, causing swelling of the endolymphatic membrane.
In the photo below, you can see two distinct colors. The first is the brown color – that is the bony labyrinth – this depicts where perilymph, the fluid high in potassium, resides. The pinker color illustrates where the endolymph is. Not pictured is the endolymphatic sac, a large protrusion toward the semicircular canals, that acts as a residual area for endolymph to swell. This swelling can push up against the vestibular nerve, causing hearing loss and dizziness. Additionally, the swelling due to an imbalance, that is not corrected quickly, can cause BPPV.

Why Benign Paroxysmal Positional Vertigo?
BPPV and Endolymphatic hydrops are related because the pressure fluctuation that happens during an episode of Endolymphatic Hydrops causes the otoconia to fall ‘out’ of the organs where they belong. There is not a lot of research that has been done to back up this information. There is some info, which I will cite throughout the rest of this article, but nothing that is totally evidence-based to back up this information. However, anecdotally, I see this quite frequently in my practice, and many other clinicians do as well, and there are a few theories.

Evidence for BPPV in Patients with Meniere’s Disease
This article, is a case review of 162 people, 9 of whom absolutely have Meniere’s Disease and the remaining had some reason to believe they did. This article only focuses on the 9 people with absolute Meniere’s Disease diagnoses, and within those 9 people, all had BPPV affect their ear, and one bilaterally. This shows that when you have Meniere’s Disease you’re more likely to have BPPV in that affected ear.
This article states two important pieces of information. The first is that most of the time, people who get BPPV have no underlying ear condition – it just happens at random. This is good because it really decreases the number of people we need to consider having vestibular conditions. However, it also states an important fact, which is that people who do have underlying vestibular conditions are more likely to have BPPV. It’s important to recognize this because knowing that you may have BPPV can make it less frightening if and when it happens. Additionally, it also states that inner ear diseases can indeed be to blame for detaching otoconia from where they belong.
The last article I will mention here is the closest I can find to solid research, rather than case studies, on this issue. This article talks about the different vestibular pathologies causing BPPV and the likelihood that BPPV is caused by a primary vestibular disorder, which in this case is referred to as Secondary BPPV. Secondary BPPV is likely underdiagnosed in comparison to Primary BPPV. This is because we often just treat the BPPV with an Epley, or other, maneuver and then not look into it further, even when it is recurring. However, if your BPPV is recurring, it’s so important to look deeper into how you could prevent this.
How do We Prevent BPPV?
Secondary BPPV is the term used to describe BPPV that’s occurring because of an underlying condition. By definition, your vestibular condition must be on the same side as where you have BPPV. So, if you have Meniere’s Disease, you’re more likely to have BPPV on the side where your Meniere’s Disease is as well. The same thing goes for Secondary Endolymphatic Hydrops, Vestibular Migraine, and Vestibular Neuritis. Preventing BPPV is not really possible in primary BPPV, because by definition it happens for no reason, but if there is a relationship between Meniere’s Disease, Secondary Endolymphatic Hydrops, or another vestibular condition you may have control over this.
Secondary Endolymphatic Hydrops is different from Primary (AKA Meniere’s Disease) because it is more predictable and not as degenerative as Meniere’s Disease. Preventing a flare of either though can be a challenge. Here are some tips:
Meniere’s Disease Prevention:
- Eat a low sodium diet
- Eat a low sugar diet
- Avoid caffeine
- Avoid alcohol
- Exercise regularly
- Medication
- Stay hydrated
- Track the weather patterns
Secondary Endolymphatic Hydrops:
- All of the above, but track your triggers
- Tracking your triggers is important with Secondary Endolymphatic Hydrops as you will be able to see what flares up your vestibular system most.
- Check in about allergies
Again, Secondary Endolymphatic Hydrops is simpler to control than Meniere’s Disease, and although not simple, tracking your triggers will help you determine what may be causing the recurrent BPPV.
Other Causes of Secondary BPPV:
Vestibular Migraine: “the prevalence of migraine in patients with BPPV was twice as high as that in age- and sex-matched controls”
Vestibular Neuritis: “The incidence of vestibular neuritis among BPPV patients has been reported within the wide range of 0.8–24.1%”