Managing Anxiety and Stress to Help Dizziness
Your head spins, the room seems to sway, and suddenly, your heart races. If you’ve ever felt this, you’re not alone. Anxiety and stress can make dizziness worse. However, understanding the connection between anxiety and dizziness and learning coping strategies can greatly alleviate its impact on your daily life.
Overview: Dizzy Anxious Cycle
The dizzy anxious cycle is so important in learning about and addressing for best results and management. This can be a ‘chicken or the egg’ scenario, but dizziness can bring on anxiety, anxiety can make dizziness worse, worsening dizziness makes anxiety worsen and on and on this cycle can spiral. Working on breaking this cycle can be a game changer for dizziness. This can be done a variety of ways and different professionals to assist. More on the dizzy anxious cycle in a blog here, or podcast here.

Overview: Dizziness and Stress
Stress has a tendency to act like gasoline on a fire. Now there is such a thing as good stress. Lifting weights or running faster/longer distances are technically stress to the body, but helps promote adaptations and progress in a way that benefits the body long term when done correctly. Good or bad, stress can take a toll on the body, especially when the body is under more stress than it can tolerate.
Dizziness and worsening symptoms adds stress to the body, making it hard to tolerate other stressors. Some stress we can be in control of, other times source of stressors are outside our control. Learning how to manage stress, especially stress outside our control, is important part of dizziness progress and management. Learning how to react to stress creates a ripple effect through emotions, attitude/mindset, and actions.
Overview: Depression and Grieving with Dizziness
While taking time to talk about anxiety and stress, depression or grief may be mixed in with these other emotions. Dizziness can be accompanied with feelings of depression, loss, and mourning of “life before dizziness”. These feelings are valid and real and should be processed in order to find coping strategies and work towards growth. This may need to be done with professional guidance. Check out this website to help find a mental health therapist to work with.
Managing Anxiety and Stress
Thankfully, there are effective coping strategies to manage anxiety and stress. Drawing insights from the Anxiety and Depression Association of America (ADAA), as well as anecdotal advice from other vestibular warriors and vestibular therapists, here are some practical tips to regain control:
- Breathwork
- Grounding
- Mindfulness
- Movement/Exercise
- The Basics
- Professional Help (linked here is another source to help find professional help)
We’ll get into the specifics below with examples of each.
1.Breathwork: There are a variety of breathing techniques that can help with relaxation. The goal of these techniques is to tap into the “rest and digest” part of our nervous system and help turn off the fight or flight system. Finding what works best for you is the goal. Deep, slow breaths is the goal.
Some examples are: yoga breathing, box breathing, triangle breathing, alternating nostril breathing, physiologic sigh etc.
2. Grounding Grounding is aimed to help anchor you to the present moment. This is helpful when not feeling connected to ones body and feeling disassociated.
Try the 5-4-3-2-1 method: identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste.
Another example is the 5 sense: something you can smell, see, hear, taste, touch.
3.Mindfulness: practicing mindfulness focuses on the present moment similar to grounding, but focusing on self awareness to help diminish sensations and promote relaxation. There are a few ways to do this and guidance can be helpful! Some examples include: EFT Tapping, Somatic Tracking, guided meditations. All offered in Vestibular Group Fit and interviews to learn more!
4.Movement/Exercise: Exercise and movement has many health benefits but has vestibular benefits as well. Exercise can help with stress, anxiety, depression, improved sleep, improved energy, reduce migraine attacks, and help build repetition and tolerance to daily movements. Progressing and scaling exercise has many benefits and translation to daily activities that are challenging. Talk to your doctor for clearance for exercise and consider consulting a provider to assist with progressing movement!
5.The Basics: Good and consistent sleep, proper hydration, healthy well balanced meals/snacks are relatively immediate and low cost changes to make in daily routines. This provides foundation for the body to have space for recovery and resources to help dedicate to recovery. Lots more on this in Vestibular Group Fit.
6.Professional Help: It takes many professionals that are experts in their own area to best assist and give tools for management. Finding the right profession, and then the right provider can be challenging, and one reason having a community for support and ask for recommendations can help find the right profession and provider faster. Someone like a headache specialist, neurologist with vestibular condition experience, or a vestibular practitioner can help!
In Conclusion
Living with anxiety-induced dizziness can be challenging, but it doesn’t have to define your life. By implementing these coping strategies and seeking support when needed, you can reclaim control over your well-being. Remember, it’s okay to ask for help, and you’re not alone in your journey toward managing anxiety in an effort to manage dizziness. Embrace these coping techniques, and empower yourself to thrive despite the challenges.
Incorporating these coping strategies into your daily routine can help alleviate anxiety and stress; ultimately helping with dizziness and empowering you to navigate life with greater confidence and resilience.
Want to learn more about mindset strategies to assist with managing anxiety and stress, as well as other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Sources
“Tips and Strategies to Manage Anxiety and Stress.” Anxiety and Depression Association of America, ADAA, adaa.org/tips. Accessed 22 Apr. 2024.
Coping with dizziness and vertigo
Dizziness can be a disconcerting and often debilitating sensation, especially when it strikes unexpectedly. Coping with dizziness and vertigo can be done through a variety of ways including lifestyle changes, medications, medical and holistic interventions.
While medical interventions and treatments play a crucial role in managing dizziness, incorporating lifestyle modifications can also be incredibly beneficial. By making simple yet effective changes to our daily routines and habits, we can better cope with and reduce the frequency of dizzy spells.
Understanding dizziness
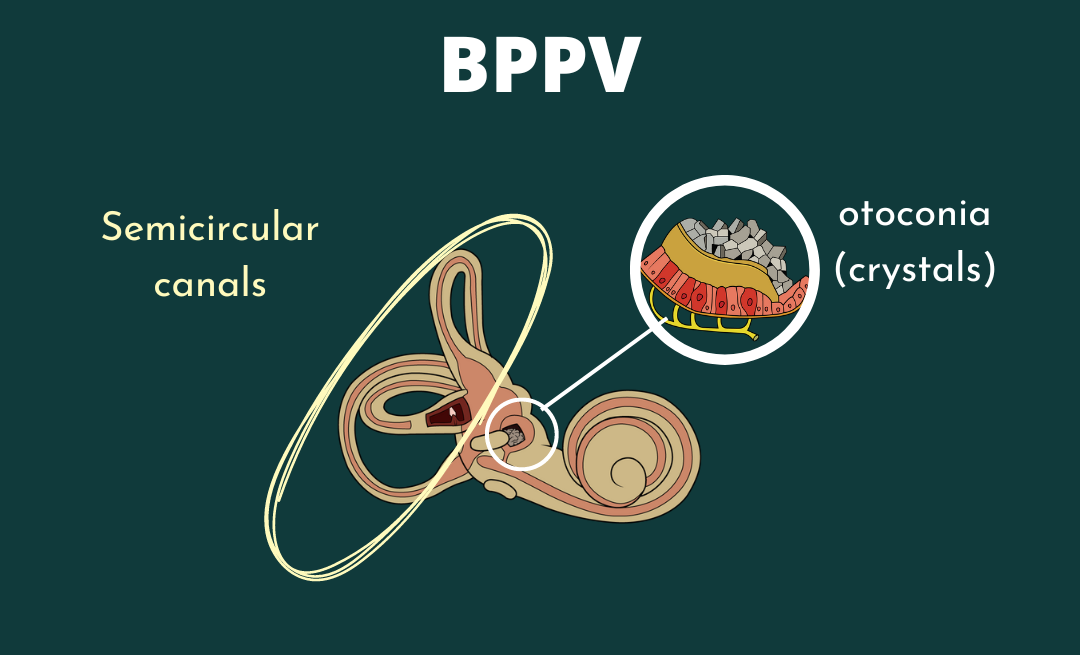
Before discussing methods for coping with dizziness and vertigo, we’ll do a brief overview of dizziness and vestibular conditions. If you’d like to learn more, this blog post goes into more detail. Vestibular conditions can result in symptoms of dizziness and vertigo as well as: light headedness, bouncing vision, rocking, swaying, brain fog. Secondary symptoms can also include anxiety, fear, depression, fear to leave the home. More on symptoms, anatomy and triggers for symptoms here.
Vestibular conditions result in inaccurate, incorrect, or delayed relaying of information to the brain. The brain takes in information from the vestibular system, visual system and proprioceptive system to determine where the body is in space, and any corrections needed in order to stay safe. If there is a mismatch in signaling, the error signal produces unwanted symptoms. Since we are dealing with spatial orientation and movement, many find quick movements, repetitive movements, or general balance to be challenging and aggravating.
It’s normal to having additional testing to rule out other causes such as medication toxicity, stroke, MS, cardiac involvement, POTS etc. There are tests to help determine vestibular involvement through ENT/audiology or with a physical therapist. More on this here and here.
Identifying the underlying cause of your dizziness is crucial for effective management.
Coping with dizziness and vertigo
Back to the Basics: these areas are probably something we’ve all been told to help support healthy habits and support the body. Many are low cost or free and tend to be overlooked at the impact they can have.
-
- Hydration. Up to 75% of Americans are chronically dehydrated(1). Limiting caffeine and alcohol, and talking to your doctor about electrolytes to assist with improving hydration can be helpful for dizziness.
- Diet. Aim for a balanced diet with fresh fruits, vegetables, grains, fats and protein. Reducing processed foods and inflammatory foods can help with gut health which can be beneficial overall and help with dizziness.
- Sleep. Consistent, good quality sleep is so important. A bad night sleep can make the healthiest person feel subpar. Getting enough sleep and regular sleep becomes even more important with vestibular conditions.
- Stress/Mindset. Working on mindfulness to help with stress and outlook has been a game changer for many with dizziness in getting back to their favorite activities or getting over a plateau. There’s a lot of resources and different ways to practice mindset, many are compiled for you and regularly updated in Vestibular Group Fit.
- Movement. There are many benefits to exercise for health, stress management, improved sleep, but can also help with dizziness. Exercise can help reduce migraine attacks and can also help work on functional strength and movements to return to activities. Starting gradual and slow is important, and is recommended to talk to your doctor and physical therapist for further guidance to get started.
Research has shown that the top 3 stressors for those with migraine attacks are sleep, stress and fatigue (2). When thinking of vestibular migraine or vestibular conditions in general, these are huge in long term management for not just dizziness, but overall well being.
Additional considerations for coping with dizziness and vertigo
- Modifications. The goal is to return to daily activities, work and hobbies to ones fullest potential. In the meantime, making modifications is helpful not only in progressing towards goals, but participating in activities with reduced symptoms. This might include breaking down tasks throughout the day, prioritizing the main tasks, taking breaks. Other options include blue light glasses such as avulux to help with screens and overhead lights. If traveling a lot or experiencing altitude changes using earplanes, or tracking weather changes with weather X app.
- Supplements. Depending on the vestibular condition, certain supplements have been backed by research to help improve symptoms.
- Support. It takes a village. Having close friends be able to help during symptom flares. A medical team to assist with treatment, tests, and ongoing management. Mental health therapists to help with coping strategies for stress or anxiety. Finding others that understand your challenges due to having vestibular conditions themselves. Having a trusted circle is so important to celebrate the wins, and support during the set backs.
- Medical intervention. This may include medications to help prevent or abort an attack from starting. This may also include vestibular rehab to work on return to movements and daily activities. Headache specialists are helpful in mangement and diagnosing of vestibular migraine. Check out this provider look up tool here. If there isn’t one close by or you have a provider you trust and is open to a collaborative team approach, consider neurahealth for telehealth appointments with headache specialists that are well versed in vestibular conditions. Click here to learn more and use VERTIGODOCTOR15 for a discount!
Remember, small changes can yield significant results, empowering you to live life to the fullest despite the challenges of dizziness.
Disclaimer
Want to learn more about management strategies and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources
- Taylor K, Jones EB. Adult Dehydration. 2022 Oct 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 32310416.
- Park JW, Chu MK, Kim JM, Park SG, Cho SJ. Analysis of Trigger Factors in Episodic Migraineurs Using a Smartphone Headache Diary Applications. PLoS One. 2016 Feb 22;11(2):e0149577. doi: 10.1371/journal.pone.0149577. PMID: 26901341; PMCID: PMC4764678.
Ask yourself: How do I support my body today?
In the fast-paced and demanding landscape of modern life, the importance of self-support cannot be overstated. As we navigate various responsibilities, stressors, and challenges, it becomes imperative to establish a daily routine centered around the question, “How can I support myself today?” This article explores the multifaceted aspects of self-support, offering a comprehensive guide on how to nourish your body, mind, and spirit each day. From mindful practices to nutritional choices, the journey of self-support is not just a daily ritual; it’s a commitment to holistic well-being.
Mindful practices for mental well-being
Daily reflection and intention setting
Begin your day with a moment of reflection. Ask yourself, “How can I support myself today?” This simple yet powerful question sets the tone for mindful living. Take a few minutes to center yourself, acknowledge your feelings, and set positive intentions for the day ahead. This practice cultivates self-awareness and helps you approach the day with a proactive and intentional mindset.
Incorporating mindfulness meditation
Mindfulness meditation is a transformative practice that supports mental well-being. Carve out time each day for mindfulness meditation, whether it’s a short guided session or a moment of focused breathing. This practice enhances self-awareness, reduces stress, and fosters a sense of inner calm. As you ask yourself, “How can I support myself today?” weaving mindfulness into your routine becomes a cornerstone of mental resilience. You may weave this into your general daily routine, or make it a specific meditative practice (We have quite a few of these in VGFit!
Journaling for emotional release
Emotional well-being is a crucial aspect of self-support. Consider maintaining a daily journal to express your thoughts, feelings, and gratitude. The act of journaling provides a healthy outlet for emotional release, allowing you to process experiences and gain insights into your emotional landscape. This practice aligns with the daily inquiry of self-support, encouraging a continuous dialogue with yourself.
Physical nourishment and support
Prioritizing nutrient-rich foods
Nutrition plays a pivotal role in supporting your body each day. As you ponder the question, “How can I support myself today?” consider the impact of your dietary choices. Prioritize nutrient-dense foods such as fruits, vegetables, whole grains, and lean proteins. These foods provide essential vitamins and minerals that contribute to overall well-being, energy levels, and immune function. If you are in the holiday challenge, comment that you read this article for 2 points!
Staying hydrated for optimal function
Hydration is often overlooked but is fundamental to supporting your body’s functions. Make a conscious effort to drink an adequate amount of water each day. Proper hydration aids digestion, improves cognitive function, and supports joint health. Asking yourself, “How can I support myself today?” includes recognizing the role of hydration in maintaining your body’s vitality. In fact, if you are dehydarted, and most people are, you can present dizzier and more imbalanced than someone who is hydrated.
Regular exercise for physical vitality
Physical activity is a cornerstone of self-support. Engage in regular exercise that aligns with your preferences and fitness level. Whether it’s a brisk walk, a yoga session, or a high-intensity workout, exercise contributes to cardiovascular health, enhances mood through the release of endorphins, and promotes overall physical vitality. Integrating movement into your daily routine is a powerful response to the question of self-support. If you feel like you can’t exercise because you’re dizzy, Vestibular Group Fit is here to help – totally safe workouts deigned for vestibular warriors every single weekday! Join us here.
Cultivating emotional resilience
Setting boundaries for emotional well-being
Establishing healthy boundaries is an integral part of supporting yourself emotionally. Reflect on your commitments and relationships, and be mindful of your limits. Saying ‘no’ when necessary is an act of self-care. By recognizing your emotional boundaries and communicating them effectively, you create a supportive environment that honors your emotional well-being.
Seeking social support and connection
Human connection is a fundamental aspect of emotional resilience. Foster meaningful relationships and seek support from friends, family, or a support network. Share your thoughts and feelings, and be receptive to the support offered by others. By building and maintaining social connections, you create a strong emotional foundation that bolsters your ability to navigate life’s challenges.
Practicing self-compassion
Self-compassion is the art of treating yourself with kindness and understanding, especially in the face of difficulties. As you contemplate how to support yourself each day, integrate self-compassion into your mindset. Acknowledge your imperfections without judgment, and cultivate a compassionate inner dialogue. This practice enhances emotional resilience, fosters a positive self-image, and contributes to overall well-being.
Balancing work and rest
Time management for productivity and relaxation
Balancing work and rest is crucial for sustained well-being. Evaluate your daily schedule and prioritize tasks based on importance and urgency. Allocate dedicated time for work, but also ensure you schedule periods for relaxation and leisure. Striking a balance between productivity and downtime is an essential aspect of self-support. Practice saying no in the mirror (yes, really!!), it will help over time.
Quality sleep as a pillar of well-being
Quality sleep is a non-negotiable component of daily self-support. Prioritize a consistent sleep schedule and create a sleep-friendly environment. The rejuvenating effects of adequate sleep extend beyond physical health; they positively impact cognitive function, mood regulation, and overall resilience to stress. Answering the question of self-support involves recognizing the profound importance of restorative sleep
Mindful rest and recreation
In addition to sleep, incorporate mindful rest and recreation into your daily routine. Engage in activities that bring joy, relaxation, and fulfillment. Whether it’s reading a book, practicing a hobby, or spending time in nature, these moments of intentional leisure contribute to a well-rounded approach to self-support.
Supporting yourself each day is a dynamic and holistic endeavor that encompasses mental, emotional, and physical well-being. By consistently asking, “How can I support myself today?” and implementing the practices outlined in this guide, you embark on a journey of self-nurturing that transcends daily routine—it becomes a philosophy of intentional living. As you weave mindfulness, nutrition, movement, emotional resilience, and rest into your daily life, the cumulative effect is a flourishing sense of well-being that empowers you to navigate life’s challenges with grace and vitality.
If this is something you’re interested in getting more help with, Vestibular Group Fit is here to help!
Why we should practice daily gratitude for dizziness
In the hustle and bustle of our daily lives, it’s easy to get caught up in the chaos and lose sight of the positive aspects that surround us, especially when we are managing a chronic illness like a vestibular disorder. Amidst the challenges, stressors, and uncertainties, practicing daily gratitude emerges as a powerful tool to foster a mindset of appreciation and unlock a cascade of benefits for our mental, emotional, and physical well-being. Additionally, recent studies have suggested that incorporating gratitude into daily life may offer unique advantages for individuals dealing with chronic illness and dizziness, making this practice even more compelling for those facing health challenges.
The neuroscience of gratitude
Rewiring the brain for positivity
Research in neuroscience has shown that the brain is malleable, and its structure can be influenced by our thoughts and behaviors. When we engage in a daily gratitude practice, we are essentially rewiring our brains to focus on the positive aspects of life. This not only promotes emotional well-being but may also have implications for individuals dealing with chronic illness, where maintaining a positive mindset can contribute to overall coping strategies and improved quality of life. Additionally, for those experiencing dizziness, the positive neural changes induced by gratitude may play a role in stabilizing the emotional response to physical symptoms, and reduce the number of physical symptoms we may experience.
The role of neurotransmitters in gratitude
Gratitude has been linked to the release of neurotransmitters such as dopamine and serotonin, commonly associated with feelings of pleasure and happiness. For individuals with chronic illness, the neurochemical impact of gratitude may offer a natural and accessible way to elevate mood and potentially alleviate symptoms of anxiety or depression. Similarly, for those grappling with chronic dizziness, the release of these neurotransmitters could contribute to a an easier shift in emotions from negative to neutral or positive, which may positively influence the perception and experience of dizziness.
Gratitude and the stress response
Chronic stress is a pervasive challenge in modern society, and its detrimental effects on health are well-documented. Engaging in a daily gratitude practice has been found to modulate the body’s stress response. For individuals with chronic illness, managing stress is often a crucial component of their overall well-being, and the stress-reducing effects of gratitude can be particularly beneficial. Additionally, for those experiencing dizziness, which can be exacerbated by stress, gratitude may act as a protective factor, helping to mitigate the impact of stress on both mental and physical health – as well as chronic dizzy symptoms themselves.
Cultivating emotional resilience through gratitude
Shifting perspectives in adversity
Life is filled with ups and downs, and our ability to navigate challenges depends, in part, on our mindset. Gratitude acts as a powerful tool for shifting perspectives, especially in the face of adversity. For individuals dealing with chronic illness, the ability to find moments of gratitude can provide a sense of control and agency, fostering emotional resilience in the midst of health-related challenges. Similarly, for those experiencing dizziness, cultivating a positive perspective through a regular gratitude practice may contribute to a solid emotional foundation in the face of physical symptoms, which makes resilience in light of an attack easier. No, it’s never ‘easy’ but we do want to build a toolkit of ways to make it easier overall. Gratitude practices help!
Fostering connection and social support
Gratitude is not always an individual practice; it has the remarkable ability to strengthen social bonds and foster a sense of community. For individuals with chronic illness, the support of friends and family is often integral to their journey. Expressing gratitude within these relationships can deepen connections and provide a robust social support system. Likewise, for those dealing with dizziness, a supportive social environment cultivated through gratitude may serve as a crucial pillar in managing the emotional and practical aspects of their condition. For example, working with your loved ones on how they can specifically help you during attacks, practicing gratitude when they help, and also helping others in your life while they are grateful for your help. This is a multidirectional relationship and help can be both given and received; and the practice of gratitude goes both ways.
Gratitude as a coping mechanism
In times of crisis or personal struggle, the practice of gratitude serves as a coping mechanism. For individuals with chronic illness, navigating the emotional toll of their condition requires adaptive coping strategies, and gratitude can provide a constructive and empowering outlet. Similarly, for those experiencing dizziness, integrating gratitude into their coping toolkit may be a part of a holistic approach to managing the emotional challenges associated with the unpredictability of their symptoms. Gratitude becomes a psychological anchor during challenging times, helping individuals with chronic illness and dizziness to weather the storms of their respective health journeys with greater resilience.
The holistic impact on well-being
Gratitude and physical health
The mind-body connection is a well-established concept, and the impact of gratitude extends beyond the realm of mental and emotional well-being. For individuals with chronic illness, maintaining physical health is often a delicate balance, and gratitude practices have been associated with improved immune function and better sleep quality. Similarly, for those experiencing dizziness, the potential positive impact on physical health through gratitude may contribute to an overall sense of well-being and gratitude for their own bodies. For example, on the days where you’re feeling better it’s often helpful to thank your body for what it did that day! After moving your body, or doing an activity, or just after a long day shifting from ‘I feel so tired, I can’t believe my body can’t do as much as it used to,’ to ‘I am grateful for what my body was able to do today’ can be very impactful.
Gratitude and personal growth
A daily gratitude practice is not merely a tool for maintaining the status quo; it serves as a catalyst for personal growth and self-improvement. For individuals with chronic illness, the journey is often marked by continuous learning and adaptation. Gratitude becomes a vehicle for embracing change, learning from experiences, and evolving into a stronger, more resilient self. For those dealing with dizziness, the practice of gratitude may encourage a growth-oriented mindset, empowering them to navigate the challenges of their condition with a sense of purpose and self-discovery.
Creating a gratitude ritual: practical tips for daily practice
To harness the transformative power of gratitude, it’s essential to establish a consistent and intentional daily practice. For individuals dealing with chronic illness and dizziness, the incorporation of gratitude into daily routines provides a structured approach to managing the emotional and physical aspects of their health journey. From keeping a gratitude journal to expressing appreciation in relationships, these actionable steps empower individuals to make gratitude an integral part of their lives, offering a practical and holistic approach to well-being. By demystifying the process and offering practical guidance, this section aims to inspire readers, including those facing health challenges, to embark on their own gratitude journey.
The practice of daily gratitude transcends a mere habit; it becomes a catalyst for profound transformation in our lives. From rewiring the neural pathways in our brains to fostering emotional resilience and contributing to holistic well-being, gratitude emerges as a powerful force that can positively impact every facet of our existence. As we navigate the complexities of modern life, cultivating a daily gratitude practice offers a simple yet potent tool for unlocking joy, resilience, and an enduring sense of fulfillment.
Did you make it to the end of this article? Comment on the Facebook Post your favorite tip for gratitude, or reason to practice gratitude, for 2 extra bonus points!
Meet marina, founder of parent with migraine
Learn how to approach parenting with chronic illness to tackle high symptom days, address parenting guilt and find acceptance with founder of Parenting with Migraine, Marina Medved-Lentini. Through her own personal experience she has created a platform to offer support, resources and guidance for other parents facing similar challenges.
Website is: here or you can copy and paste into your browser: https://parentingwithmigraine.com/
Instagram: @parentingwithmigraine here.
Marina has been living with migraine disease throughout her life. Her migraine attacks were episodic during her teenage years and through college and law school. After becoming a parent, Marina began to experience chronic migraine. Finding migraine support groups on social media helped Marina find hope, support, and information to work with her medical team to get her migraine managed. Her experience has motivated her to share her knowledge with others and become a migraine advocate. In vestibular group fit, Marina and Dr. Madison talk about screen time, parent guild, ways to prep and adapt when parenting with chronic illness.
Parenting with Chronic Illness Tip: Parent Guilt
Parent guilt can come in feelings of inadequacy, guilt of missing out on precious moments, or not feeling present or providing enough for your family. We tend to be our own biggest critic, and it’s important to look at these thoughts and feelings to determine what might be stemming from self doubt or own inner critic.
Having a chronic illness doesn’t define you. Parenting with chronic illness doesn’t define your value as a parent. You are strong and your provide your own set of strength and perspective as a result of your lived experience, chronic illness included.
Tips to help combat parent guilt:
- don’t compare yourself to others. social media can create unrealistic expectations. If your kids are happy and have what they need, that’s what matters! Marina shares her realization that kids want to feel included in your life and this can be done with simple connections like watching a movie together. It doesn’t have to be an elaborate social media activity.
- be kind to yourself. What would you say if this was your best friend having thoughts of self doubt? Is that what you’re telling yourself, or is your harsh inner critic talking?
- Doing your best is what counts. It’s okay to ask for help. If friends or family have shown interest in helping, take them up on it. A little help can go a long way.
- Get support! finding a community of those who share similar experiences and struggles can create a space to share openly your thoughts and feelings. You’re not alone in this.
Sometimes parent guilt comes in the form of potentially passing on a chronic illness such as migraine to your child. Migraine disease does have a hereditary component. Knowing about the signs and symptoms of your chronic illness in children can help identify the need for intervention quickly. Remember, there is so much more to a child than a chronic illness. Kids are resilient and have repeatedly reminded me that there’s something to be excited about and get the most out of life.
In the case of pediatric migraine, Marina shares resources on learning signs and symptom of migraine in kids to help get them proper resources. Migraine at school is a great resources for parents, educators and how to help support students. check them out here!
Parenting with chronic illness tip: preparedness and adaptability
Part of parenting is having to be flexible and adapt to changing situations. This is even more true when parenting with chronic illness. Having some items prepared can help on days when you’re not feeling your best. check out some tips below.
- Talk to your children about your chronic illness. It doesn’t have to be super in depth, but at a level they can understand. Answer any questions they have. Being honest with your kids can help them understand more of what’s going on if you’re not feeling well, instead of potentially catastrophizing the situation into a worse case scenario in their minds.
- As kids get older, they may benefit from having a role to help support you. This might be grabbing an ice pack or a migraine kit for you. Maybe it’s brainstorming a list of activities they can engage in more individually or next to you that are better tolerated when you’re not feeling your best.

Parenting with chronic illness tip: acceptance
Finding acceptance and self compassion has been noted by many as a main part of living with a chronic illness. Acceptance doesn’t mean you’re giving up but learning to live with a chronic illness. This includes finding ways for best management while coming up with solutions to keep doing your everyday. Your plan for you day might change or look completely different than you expected and that’s okay! Acceptance helps us address the stress and change of the unknown. We cover this more in our self compassion blog and premium content in vestibular group fit and more on acceptance in this blog post.
Disclaimer
Want to learn more about how to parenting with chronic illness, household tasks and social situations and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Learn tips for dating with a vestibular disorder. We cover dating, relationships and intimacy with Dateability cofounder Jacqueline Child.
Dateability: A Dating app for those with disabilities and chronic illnesses.
Dating with a vestibular disorder can be challenging or intimidating to begin after a receiving a vestibular diagnosis. Jacqueline Child is a co-founder of Dateability and talks with Dr. Madison oak about dating and intimacy with chronic illness and disabilities. Jacqueline encountered ableism on other dating apps, and experiences impacting her self esteem. In october 2021 after a feed tube surgery, Jacqueline expressed her wish for a dating app tailored to people like herself. Jacqueline’s sister proposed they make this wish a reality. Dateability aims to foster understanding, compassion and connection to provide a safe space where chronic illness is not a deterrent to finding meaningful connections and love. Learn more about this app here.

5 Suggestions when dating with a vestibular disorder
1.You’re more than your vestibular condition! Talk about other interests, projects or hobbies you have going on or hope to start!
2. Explaining your vestibular condition can be short and simple at first. Jacqueline compares it to how you’d explain your condition to a child. Remember, you’ve learned so much about your condition, that it can be overwhelming to someone that is learning. This can vary based on their exposure to the medical field as well (vocabulary and health literacy etc). Keep it easy, if they have follow up questions and you want to answer them, go for it!
3.If there’s an activity that doesn’t work great for you, let your needs known and suggest an alternative activity. When dating with a vestibular disorder, certain activities might not be the best for you. Instead of saying no to their suggestion, feel free to let me know that won’t work for you and suggest an alternative activity that works for you. For example swap out a bike ride for a picnic in a park, or maybe a tram bike that moves slower and multiple people steer and peddle.
4.Be honest about your needs early on. You don’t have to list them all out day 1, but when something comes up, mention the relevant information or accommodations needed. For example, if someone suggests a movie and the time is late. Casually mention that staying up late isn’t great for you, and see if the there’s an earlier showing.
5.Communication is key when dating with a vestibular disorder, and discussing your vestibular condition is a very vulnerable thing to do. Practice can help, whether it be with close friends and family, or going on some dates just to practice how you share your story with someone new.

Tips for Discussing Chronic illness in Dating or with your current partner
- Communication is so important. Be honest about how you’re feeling, and limitations.
- not communicating your feelings and needs is unfair to yourself and your partner. Expressing your feelings and needs is the best way for others to understand what’s going on. Assuming others can read your mind can make everyone frustrated.
- hiding symptoms and pushing beyond your limits to appease others ends up backfiring in the end
- Have a codeword or phrase to convey you’re not feeling well. It lets other know what you’re feeling without having to put it into so many words.
- Longer conversations and explanations might not be necessary at first. But can be beneficial to have eventually to ensure understanding, trust, and building a deeper connection.

Navigating intimacy with vestibular disorders
Intimacy and sex is an area that is important to address when it comes to dating with a vestibular condition and relationships. This part of romantic relationships can be a source of apprehension when dating or looking for a long-term partner. Communication here is so important (sensing a theme about communication?).
Having a conversation outside of intimacy and sex can help. Knowing modifications or positions that are best, or how to handle situations when a pause is needed beforehand will help in the moment to do what’s best for your body. This may feel uncomfortable or awkward, but communication is about trust, and knowing your partner cares about you to support you and want what’s best for you in all aspects of life.
Disclaimer
Want to learn more about dating, relationships, other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
EFT tapping for dizziness
EFT or Tapping is a free and easy way to address unpleasant experiences, emotions, memories and you guess it, dizziness! EFT practitioner Rochelle Schulz dives into what EFT is, the benefits and how to do it anywhere.
Meet EFT practitioner Rochelle Schulz

Rochelle Schulz is an EFT practitioner offering internationally accredited and certified services. With a focus on trauma-informed training, she creates a safe and non-judgmental space for adult individuals worldwide, both in-person and online.
Rochelle’s goal is to assist clients in healing, personal growth, and regaining confidence. By delving into the subconscious mind, we uncover and release patterns that have been running in the background, including traumas, phobias, cravings, and physical pain. Working together, Rochelle’s clients can reclaim their authentic selves and experience a life of meaning, joy, and purpose.
Rochelle Schulz specializes in guiding clients through uncomfortable emotions and facilitating a smooth journey for their brain and nervous system, minimizing dysregulation.
Here website is linked here to learn more about Rochelle’s services and offerings. She assist with individuals, group sessions, creating scripts to use on your own tapping sessions, free consultations and more!
What is Emotional Freedom Techniques (EFT Tapping)
EFT or tapping has been around since the 1970s and involves tapping with your fingers on different pressure points on the body. These pressure points are the same ones used in acupuncture but without the needles. Rochelle notes that EFT is an effect strategy for stress relief, boost immune system function, and turn off genes related to chronic illness.
EFT combines the concepts of energy pathways (meridians) rooted in acupuncture with somatic and cognitive behavior therapy to calm our nervous system and address difficult emotions and memories.
It’s effective, can be done anywhere, anytime, and you can do it yourself for free!
What is Bottom up therapy?
EFT is a bottom up therapy. Typically, when addressing dizziness, emotions, trauma etc, therapies are focusing on the head/brain. The brain is important in our experiences, but our cognition only makes up 20% of that experience. Rochelle goes on to explain that the body stores up to 80% of our experiences and memories in 4 different ways. They are:
- emotional memory
- sensory memory (hearing, sight, taste, touch)
- autonomic memory (temperature, respiratory, digestion)
- physical memory (muscle memory or movement memory)
Bottom up therapy looks to address the 80% of experiences and memories stored in our body. To process and calm our nervous system in this way, bottom up therapy is looking to address the majority of our body that other interventions ignore.
How EFT Can Be Used
EFT/Tapping can be used on three different levels:
- First aid calm down: This is used in the moment of a stressful event (traffic, hard conversations etc).
- Taming the trigger: It can help us reduce the emotional intensity of triggers. This allows us to respond calmly in the moment when this trigger is enacted.
- Trauma release: EFT can address deep-seated beliefs and traumas from our past that may affect our self-perception and behavior as adults.
EFT aims to find the root cause of limiting beliefs or traumas and release them, allowing us to let go of old programming, retrain our brain to have positive neural pathways, and live more freely. EFT tapping for dizziness can help break the dizzy anxious cycle, find acceptance, and retrain our body/brain neural connections for long term results. This takes time and practice!
Common Accupressure Points used in EFT Tapping
Using one or both hands, listed below are acupressure points used in EFT/Tapping.
- Side of the hand between the bottom of your palm and start of your pinky finger
- eyebrow
- side of the eye (near the temple but want to be on the firm/bone part, NOT the soft part)
- under the eye
- under the nose
- chin/under the mouth
- collarbone
- under the arm (4 inches below the armpit). You can reach across your body to tap this area or use tap on the same hand/under the arm if it’s comfortable to you.
- top of the head
Considerations for EFT tapping for dizziness
Some find that areas by the eyes or peripheral vision increased dizziness. If you notice this, choose tapping points that feel best to you (collar bone, under the arms, top of the head etc). Sometimes eyes closed or laying down can help this as well.

How to do EFT Tapping for Dizziness
1. RANK THE INTENSITY
Rank the intensity of the issue on a scale of 0–10.
2. TAP ON THE SIDE OF THE HAND
Tap with 4 fingers the edge/palm of your hand, near the base of your pinky finger.
“Even though I have [insert emotion, symtpom etc] in [insert location in your body] when I think about this [feeling, memory, experience, situation], I deeply and completely accept myself.”
Allow your body to soften and relax, be present with any symptoms or discomfort. You can acknowledge sensations without needing to control them.
Thank your body for its effort to protect you and give yourself permission to receive instead of resisting.
3. TAP WITH REMINDER PHRASE
The reminder phrase should acknowledge the issue and convey self-acceptance in spite of it.
some examples are:
- I’m willing to allow these thoughts and emotions now
- I’m noticing what I’m feeling in my body
- I’m recognizing these symptoms
- I’m allowing to be with this discomfort/illness
- I’m going to tune in and be with these symptoms
- It can be scary sometimes. Even though I think I need to control this. I can still soften anyway.
- I’m thanking my body for trying to protect me in some way.
- I give myself permission to receive instead of resist; these sensations that are happening now.
Using two or more fingertips, tap approximately 5x on each point listed above for 1- 2 rounds while repeating your reminder phrase. This can change with each session, and pick the tapping points you feel best with. Avoid the ones that make you dizzy.
4. REASSESS THE INTENSITY
Rank the intensity of the issue on a scale of 0–10. Continue repeating rounds until the intensity reaches zero or plateaus.
Resources
The tapping solution has a website and a smartphone app to help learn and perform guided tapping sessions. There’s a free and paid version! Check it out here.
Work with Rochelle Schulz! She has individual, group and free consultation services. Check out her website here.
Disclaimer
Want to learn more about different benefits of various tapping points, a guided tapping session with Dr. Madison and Rochelle Schulz, other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
How to get through your ‘To Do’ List & Daily tasks with dizziness
Energy conservation (or pacing) is a way to listen to your body and strategize your day to get chores done while minimizing fatigue and dizziness as much as possible. Read on to learn how to get through your ‘to do’ list and daily tasks with dizziness, learn why it’s hard, ways to get it done today!
Phone battery analogy
Use a 0-100% battery meter to gauge your energy levels and dizziness on any given day. Keep in mind tasks you do will drain your batter, just like using your phone will drain it. Don’t let your energy battery (or phone battery) reach zero. It’s easier to charge when you’re at 70-80% than when you’re at 10%.
6 Tips & Tricks to pace with dizzness
Take a look at these 6 tips to strategize your day. Consider your energy/dizzy battery for the day and these tips to map out your day. Reminder, it’s okay to ask for help, to prep part of a task for a later day (like soaking dishes), or delegate to another family member or service.
Some days we have big plans to get things done, but we wake up with increase symptoms, fatigue, and a lower body battery. That’s okay, it’s not your fault and you are not a failure. Focus on what can be done, including self care to have the capacity for your list another time.

Household and daily tasks with dizziness: the breakdown
In this section we’ll cover some common household chores or daily tasks and discuss why they’re challenging and ways to make them easier.
Our premium content members also have guidance on movements and strength exercises to increase their tolerance to these tasks. Doing exercises and movement will make tasks easier to do in the future. Learn more here.
Dishes
Why it’s difficult:
- Repetitive body movement (from sink to rinse to drying rack)
- eye tracking
- standing balance
How to pace with dizziness:
- Use the dishwasher if available
- stack dishes to move more at once and reduce large/repetitive movements
- soak dishes to make cleaning easier and faster
- wash multiple items before rinsing to reduce movements
- try a suction glass cleaner to take some of the effort of off you.
Laundry
Why it’s difficult:
- lots of up/down movements
- busy visuals
- noise/smells/light depending on the environment
- mental energy to sort and fold
How to pace with dizziness:
- ask for help. Have family take their own pile of laundry to put away or fold
- do folding and sorting seated
- Make laundry your one task for the day. Break down the tasks to give yourself rest time
- don’t fold everything! I’ve started to keep clothes I don’t mind being wrinkly in fabric bins. When I sort laundry I can put my socks in the sock bin, delicates in the delicate bin, and workout shirts/shorts in their bin. Cuts down my laundry time and I realized how much folding I did for things that I didn’t care about needing to be folded.
Stairs
Why it’s difficult:
- physically demanding
- looking down
- visually challenging: seeing both near and far
How to pace with dizziness:
- Use the railing when available
- reduce trips by doing all tasks on the top floor and then going downstairs for tasks
- keep a basket at each end to place objects in that need to go up/down to avoid multiple trips. A great way to get others to help as well!
Cooking
Why it’s difficult:
- looking down
- balancing
- lots of turning and reaching
- tracking
- focus
How to pace with dizziness:
- use some prepped foods like pre cut veggies
- do food prep in sitting when able
- Find simple recipes, The Dizzy Cook is an awesome resource, her cookbook is here
- have some easy frozen and pre baked meals
- use a slow cooker
Computer time
Why it’s difficult:
- tracking and scanning
- head position and posture
- mental fatigue and concentration
- light sensitivity
How to pace with dizziness:
- ergonomics for better computer posture (some extra tips for set up here)
- avalux glasses (code: VERTIGODOC will you get $25 off) or other blue light blocking lenses
- taking breaks with the 20-20-20 rule
Reading
Why it’s difficult:
- mental fatigue and concentration
- tracking and scanning
- head position and posture
How to pace with dizziness:
- audiobooks when able
- use your finger to help track the line you’re reading
- take breaks
Showering, Grocery Shopping, Escalators, Elevators, the dentist/hair dresser, cleaning the house, gardening and more!
Learn why wall these tasks are challenging, ways to get these tasks done now and products that help, and how to work on movements to improve all of the tasks listed today! All of this and more is included in our supportive community at Vestibular Group Fit! Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Jaw Pain and Dizziness: 5 ways to Manage TMJ and dizziness
Jaw pain and dizziness are related and have an interesting relationship. It can be challenging to know which one causes the other. This article outlines 3 ways TMJ and dizziness are related, including TMJ and migraine, and 5 ways to help mange TMJ pain and dizziness.
What is the TMJ?
TMJ stands for “temporomandibular joint”. This is where the mandibular fossa of the temporal bone of the skull and mandibular condyle of our jaw bone meet. This makes the joint we commonly refer to as the jaw. Some may say “I have jaw pain” and point to the TMJ, others may say “I have TMJ issues”.

3 Ways TMJ Pain and Dizziness are Related
The anatomy around our jaw includes a lot of important systems that are connected to dizziness and migraine. Read below to learn how jaw pain and migraine, jaw pain and dizziness, and jaw and neck pain are related.
- The muscles around the jaw and neck can refer pain to the ear. It may feel like there’s an ear infection starting, but it might actually be tightness in jaw or neck muscles, or inflammation around the TMJ.
- Inflammation of the TMJ can influence the fluid balance of the innter ear via the eustachian tube. This can result in an imbalance of the inner ear, which can result in dizziness.
- The trigeminal nerve stems from an area very close to our ear. The trigeminal nerve is involved in current migraine theory as a contributor to migraines and is connected to vestibular migraine. The trigeminal nerve is in charge of touch, temperature and pain sensations in most of our face. Part of the trigeminal nerves involvement in migraine is facial pain or pain behind the eye that some experience during a migraine attack.
How do I know if my Jaw pain and dizziness are connected?
The best way to find out if your jaw pain and dizziness are related is during an examination. If assessment of your jaw or neck recreate your symptoms or make current symptoms worse, it is something that should be addressed in your plan to improve your dizziness. Based on other findings from your exam, there might be other areas your provider would like to address first. In some cases, as other areas improve, TMJ or neck pain may improve naturally. If other areas start to improve but you’re still noticing TMJ or neck pain, then a more focused approach should be used. It’s an important conversation to have your with your medical team and your plan may change over time, so keep having those conversations!
5 ways to address TMJ Pain and Dizziness
- Practice Tongue and jaw resting position. Your teeth should not be touching when your mouth is closed and at rest. Jaw should be relaxed. Tongue should be resting on the roof of your mouth, not on the back of your teeth.
- Avoid sleeping on stomach. This places pressure on the TMJ and can contribute to pain and inflammation.
- Avoid unnecessary jaw strain/movements (resting your head in your hand, super chewy foods like bagels, taking large bites of food, nail biting, gum chewing etc.)
- Improve posture. Posture influences our neck and head position. Good posture can help address muscle tightness or poor jaw positioning that can impact TMJ pain. Good computer posturing is a great place to start. Computer moniotor should be be at eye level, keyboard should be where your arms can relax at your sides and your elbow makes a 90 degree angle, feet supported by the floor or stool to have knees at a 90 degree angle.
- Frequent movement breaks. Getting up every 30-45 minutes for a movement break or changing positions. This will help improve posture and allow muscles a change to relax and avoid stiffness or tightness.
- See a TMJ PT or TMJ specific dentist. Click here to use this directory to see if someone is near you.
Want to learn more about TMJ assessment, surveys, and TMJ exercises and other vestibular tools to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Tips and tricks for traveling with a vestibular disorder
Travel plans can be popular this time of year to spend holidays with family and friends, warm vacation destinations, or other special occasions. Overall, no one really loves traveling, but it can be even more challenging with a vestibular condition.Read below to find some lists of our favorite travel tips with a vestibular disorder and for some specific to different travel types!
How to travel with a vestibular disorder: Preparation is key!
Here are our Top 10 effective tips to help prepare for your upcoming trip and traveling with a vestibular disorder successfully. Keep reading to learn more about how to travel with a vestibular disorder based on specific types of travel!
- Make the first planned trip low key. A short trip or close destination is a good idea to test out traveling and make adjustments for future trips.
- If staying in a condo or hotel, request a lower floor. This will help with any symptoms with heights and reduce time spent in an elevator (or just using the stairs!)
- Make sure you have enough medication prior to your trip. If your meds run out while on your trip, get a refill before travel. Talk to your doctor if it’s a controlled substance to get a plan on how you’re going to have your needed medications for your trip.
- Pack a small bag within your suitcase. This gives you something to easily carry important meds or your vestibular kit on day tips at your new destination.
- Pack a vestibular travel kit. Pack all the things you use for symptom management in one bag. Make sure this bag is easy to access throughout your travels. Store it in your personal item or carry on bag if you have one. It may include:
- Medications (rescue, preventative, over the counter etc)
- Peppermint or ginger (candy or scented oil)
- migraine/blue light glasses (we like avalux if you want to check them out here)
- Hat
- Ear plugs/noise canceling headphones
- Snacks
- Water
- Travel pillow
6. Pack your own pillow. Having your own pillow helps ensure a good nights sleep at your new destination. Some people will order and ship a pillow similar to theirs to where they are traveling to cut down on packing!
7. Stay hydrated throughout your travel day. Taking additional breaks for the bathroom can help keep you active and use it as an opportunity to check in with yourself and take a break if needed.
8. Get a good night’s sleep the night before
9. Eat a good breakfast on travel day.
10. Try to stay active before and during travel. Light walks, different position changes while sitting, seated marches, seated kicks, standing heel raises or sitting/standing can help keep your body moving.
How to travel with a vestibular disorder based on transportation (car, train, plane, boat)
Traveling with a vestibular disorder by car
Driving is a common challenge I hear when working with those who have vestibular conditions. If you’re looking for more driving tips, check out our other blog post on driving here. This list is geared more towards longer driving trips to reach your travel destination. Let’s dive into how to travel with a vestibular disorder by car:
- Pack ahead of time, if you notice something you’re using regularly, put it in your suitcase so you know you won’t forget it.
- Pack up the car the night before
- Sit in the front passenger seat, keep your eyes on the horizon
- Listen to music or audiobooks for entertainment
- If being the driver helps your symptoms, make sure you’re safe to do so! Talk to your doctor about returning to driving and make sure you practice driving for longer periods of time and learn your drive time limit.
- Use gas stops/bathroom stops as time to take a movement break and do gentle stretching, exercise or walking. Use as a time for grounding as well.
- If the drive is more than a few hours, consider flying to cut down on overall time traveling.
Traveling with a vestibular disorder by plane
Traveling by plane can be really daunting, especially after living with a vestibular condition. We at The Vertigo Doctor want you to consider flying as an option, especially if it cuts down travel time considerably. Less time spent with the stresses of traveling means the sooner you can start to rest, relax, and recover! Here are ways for traveling with a vestibular disorder by plane:
- Have your vestibular travel kit with you on the plan and easy to access in the airport and during the flight
- Give yourself plenty of time to reach your gate. Recommended time is usually 2 hours prior to your flight. If you’re not familiar with the airport, or it’s a large airport that involves shuttles, giving yourself more time to rest and ask for help can help reduce the stress of flying! If unsure, ask for help sooner rather than later!
- Try to book direct flights
- Try to avoid flying during really early or really late flights to avoid large shifts in your sleep routine
- If changing time zones, try to slowly adjust your sleep schedule by 15 minutes the days prior to gradually match your time zone if possible.
- Try to sit in the aisle and near the wings. This can help minimize any rocking from the plane and the aisle gives you ample opportunity to get up and move.
- Try to avoid smaller planes that aren’t pressurized
- A travel neck pillow or eye mask can help make yourself comfortable on the plane.
- Ear planes are ear plugs made for air travel to help with pressure changes. Yawning or gum can also help with altitude changes
- Ask doctor for any medication suggestions to help with plane (like a decongestant or rescue med if you don’t have one)
Traveling with a vestibular disorder by train
Trains might not be as common in the United States for longer trips, but these tips may help if you take a train for your daily commute. If you’re also trying to travel to another country or continent that uses trains more for travel such as Europe, check out these tips on how to travel with a vestibular disorder by train:
- Face forward and on the aisle to avoid too much visual stimuli. Looking outside tends to be more challenging.
- Take a short movement break at train stops.
- If the train is moving and you need to get up, it’s okay to use your hands to touch the chairs or overhead luggage compartments for more balance when walking on the train.
- If you have to stand, spread your feet wide to have more support, try finding a pole to hold onto to try to avoid holding your arm overhead for extended periods. If the overhead grips are the only thing available, try to alternate your arms every stop to get a rest.
Traveling with a vestibular disorder by boat
Whether it be by ferry or a an afternoon on the lake, boating is certainly a way of transportation to be prepared for! Here are some considerations when traveling with a vestibular disorder by boat:
- Sit towards the center of boat to reduce rocking
- Try to stay outside on the deck if possible.
- Talk to your doctor about any recommended motion sensitivity medication to bring in addition to your vestibular travel kit
- Sea band or acupressure bands can be helpful for some with sea sickness.
How to recover from traveling with a vestibular disorder
- Congrats on your trip!
- Remind yourself that some “off” sensation or feelings is normal for anyover after a lot of travel and it will get better.
- Try a short walk to help “reset” the system
- Get good night’s sleep
- Grounding, meditation, relaxation.
- Try to make the day after travel a calmer day. Something restful and relaxing. If you want to join a group that’s something more adventurous, try to get there a day early to recover and be ready for it!
If you found this article helpful, check out this other article on our site that has additional information on traveling with a vestibular disorder by clicking here.
Want to learn more about managing your vestibular condition with travel, return to driving, hormonal impacts, and other vestibular tools to get back to your daily life? Find out more below!
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.