Holistic Management of Vestibular Migraine with Dr. Sheikh
Dr. Sheikh is very knowledgeable and has had extensive training to help address and manage headaches, and more specifically migraines. Dr. Sheikh got her MD and then completed her residency at MOntefiore Medical Center in Bronx NY. She then went on to complete two fellowships; a vascular fellowship and then a fellowship in “Headache and Facial Pain” Harvard Medical school and is now an adjunct professor at Ichan Medical school at Mt Sinai in New York City. Being in a clinic setting for over 6 years now, Dr. Sheikh has been treating and helping her patients manage complex headaches with a holistic approach. She’s very up to date on current medication options and other complementary treatments that she is sharing with us in Vestibular Group Fit!
Migraine is more than a Headache
“I like to think of migraine as a disease, and headache as a symptom…migraine is a genetic neurological disease and headache is a symptom of migraine”. Dr. Sheikh
Migraine is more than just a headache! Migraine may have a headache (not in all cases) but also vertigo and dizziness, light or sound sensitivity, brain fog, or visual auras. Headache associated with migraine is most reported disabling symptom, but others may have dizziness or sound sensitivity as their most prominent symptom. For a more indepth look at vestibular migraine, here’s a helpful article to review, click here.
How do we treat migraine holistically?
How do we treat migraine holistically?
- Your doctor should listen
- Best management should be a discussion about your experience, your options, and creating a plan. Not just being given a prescription and nothing else. If a med is all you need and you’re interested in, great! Having the chance to discuss what you want and the options is key.
- Remember, you have options
- Don’t like the idea of medications? Meditation, diet, exercise, yoga, breathing, sleep and more can be a major part of your preventative plan. Sometimes medications are helpful in getting you feeling better to get a better foundation to manage holistically. You don’t need to be on meds forever but it can be a useful tool. Using medications is not a failure, just a tool that can be used daily, only during attacks, or never. This is why discussions are so important to address concerns and adjust your plan based on your responses for best results.
- Reducing hypersensitivity (increasing your threshold)
- Addressing your treatment holistically can reduce hypersensitivities and help increase your migraine threshold
- Treat from all angles
- Holistic and natural options are wide ranging and finding the ones that work for you can be super helpful in migraine management. Medications can range from a daily preventative, botox injections that are months apart, or an abortive med that’s only used to reduce your symptoms during a migraine.
- Stress management
- Stress can lower our migraine threshold and make you susceptible to an attack, the better we can use holistic approaches to manage stress, the better for not only your migraines but your overall well being!
- Be prepared!
- A common stressor for those with migraine is the unpredictability of when a migraine attack might occur. Having a plan in place (natural remedies, an abortive med, ice packs etc) can help reduce the stress about a possible attack, ultimately decreasing your attack frequency. Having a plan is key!
Treatment for vestibular migraines is overall similar to other migraine management, however Vestibular Rehab Therapy with a physical therapist can be helpful and neuromodulation devices (cepahly or gammacore for example) can be good options to consider when addressing vestibular migraine!
Contact info for Dr. Huma Sheikh:
Instagram: @headachesnyc
Website: Headachesnyc.com
Dr. Sheikh talks more about family planning, diet, and sleep in the premium content in Vestibular Group Fit. Found out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Long-COVID rehabilitation: The best Treatment for Long-COVID
We all were affected by the COVID-19 pandemic, and because of that we have all heard of Long-COVID, and hopefully, about Long COVID Rehabilitation. And, no matter what happened to you or around you during the pandemic, somethings has become more and more prevalent over the last few months is Long-COVID. Long-COVID is a hot topic, and I want to start off by saying one thing: You are NOT making it up. I have worked in chronic illness since I gratulated from Physical Therapy school and I understand the gaslighting in the medical system, especially the US medical system. BUT, I am here to tell you that you are making that up. Most people with the COVID-19 virus recover within 1 week, but that’s definitely not the case for everyone. According to UCLA health, one in three people with a COVID diagnosis will develop Long-COVID.
So, today let’s talk about it: what is Long COVID Rehabilitation?
Are you making up Long COVID?
You are not making it up! I want you to know that this is not in your head.
Your symptoms, whichever way you may be presenting, are very real. I have seen many providers who either ‘don’t believe you’ or ‘don’t believe Long-COVID would be so severe’. But, I am here to say that there are many different and debilitating symptoms!
The biggest issue we are having is that we don’t have enough research on covid and Long-COVID, so many provider just don’t know what to do about it at this point.
What are Long-COVID symptoms?
Long-COVID symptoms can be incredibly variable and truly span anywhere from fatigue to cardiovascular issues. Your symptoms can be cardiovascular, respiratory, general fatigue, fever, difficultly sleeping, and more. Because we just don’t know enough about Long-COVID right now, we can’t make an exact list. But, if you had COVID and now you’re experiencing symptoms you did not have before it could definitely be correlated with Long-COVID. Long COVID symptoms could last anywhere from a few weeks to years. COVID began in early 2020, and patients have been dealing with Long-COVID symptoms since that time. It’s difficult to say at this time if they last forever or not. However, it does seem like we are able to treat Long-COVID, though through LongCOVID rehabilitation and medication.
Long-COVID & Dizziness
Long-COVID is known to cause many different symptoms, as we discussed above. One of the overarching symptoms that we did not touch on above is dizziness. As a provider who treats dizziness and vertigo, I have been treating SO much Long-COVID. It started with just one patient who had dizziness related to COVID-19, but has been a very big influx of my caseload, especially for someone who treats Vestibular Migraine and PPPD usually.
Long-COVID Dizziness is thought to come from the virus infecting and inflaming your inner ear. Your inner ear controls balance and equilibrium, and spatial awareness. Without this organ functioning accurately, you will feel dizzy, light headed, and other related symptoms. Another Long-COVID dizziness diagnosis is POTS. POTS, or Postural Orthostatic Tachycardia Syndrome is an autonomic dysfunction. Autonomic dysfunction is your automatic systems in your body. Everything from digestion to heart rate and breathing are controlled by your autonomic system, because these are all involuntary. And, they’re REALLY important! Long-COVID rehabilitation, can help regardless of the type of dizziness you are experiencing after a Long-COVID diagnosis!
Long-COVID rehabilitation has had its difficulties in treatment, but it’s nothing that my patients and I haven’t been able to trouble shoot. Long-COVID is not one of those sicknesses that you get and then suddenly you just get 100% better again. There may be adaptation and compensations you have to make in your life, and your lifestyle may look a little bit different than it did pre-COVID. However, I do find that specific rehabiltation directed at each of your symptoms is incredibly effective in getting you back to at least some of your ‘normal.’
How do you treat Long-COVID?
Long-COVID is complex, and I like I said above, we just don’t know enough about it. But, we have seen that Long COVID rehabilitation is effective. Your symptoms can range anywhere from looks like POTS to seeming like a concussion. No matter what the symptoms, Long-COVID treatment is rehabilitation. Long-COVID rehabilitation providers are typically physical therapists and occupational therapists. There are also medical providers who have branched into this kind of medicine as well. There are a few studies that have shown to be somewhat effective in treatment with medication. At this time it is all preliminary information. UCLA and Stanford both have excellent West coast treatment centers. Additionally, there are a few others like in Kansas City, Germany, New York City, and more!
Treating Long-COVID from a medical standpoint and a rehabilitation standpoint is the best way to go about treatment overall. I recommend finding both a medical doctor and a physical or occupational therapist to help you rebuild strength, improve visual symptoms, reduce dizziness, and more.
Long-COVID Rehabilitation
Long-COVID rehabilitation will look like a few different kinds of physical therapy combined into one treatment plan.
At this point, there are not many experienced Long-COVID rehabilitation practitioners, none of have more than a year or so of experience. However, we all piecing together information the best that we can! If you are looking for a provider, I recommend calling around to physical therapist and occupational therapist offices and asking if they’ve had any experience working with Long-COVID rehabilitation patients. And, if there is not someone in your area, try and find someone who is at least willing to learn with you!
Currently, I am taking patients for Long-COVID rehabilitation in the following states via telehealth: Wyoming, Virginia, Maryland, California, New York, and New Jersey!
If you’d like to schedule an evaluation appointment to work with me, email me at [email protected] for more information!
Visual Vestibular Integration: Why do busy environments make me dizzy?
Our body uses three main systems to know where we are in space and what needs to be done to be balanced and safe. Today’s focus is going to be on our eyes and inner ear working together with visual vestibular integration. Let’s talk about what this is, what happens when visual vestibular integration isn’t working, and what to do about it!
If you need a refresher on our body’s main systems for balance, click here to review our What is Balance article before reading on.
What is visual vestibular integration?
Visual vestibular integration is combining the information from our eyes and inner ear to carry out tasks to help with our balance. These two systems work closely together to help keep our vision steady when moving our body, head, or both at the same time. This is known as the vestibulo-ocular reflex (VOR).
The brain also uses visual and vestibular information to gather as much information about your environment and compares all this information to get as clear a picture as possible. This creates checks and balances to ensure that our brain knows what is going on and can respond correctly.
A good example of this is when you’re sitting in a parked car. The car next to you starts to back up, and you feel like you’re moving briefly. This is your eyes picking up the car backing up next to you and saying “hey we’re moving what are we going to do about it”. You quickly realize that you aren’t moving because your vestibular system kicks in and says “actually we aren’t moving, the eyes are seeing that other car move, we are SAFE”.
If you read the previous article What is Balance, you know there’s the proprioceptive system. We do use our proprioceptive system to compare sensory information with our eyes and inner ear- especially on uneven surfaces and to make sure any body movements are accurate and correct. This relationship is not the main focus of this article but it does exist! We’re focusing on the connection between the inner ear and eyes because of certain symptoms people experience when visual vestibular integration isn’t accurate, so keep reading on to learn more.
What happens if visual vestibular integration doesn’t work?
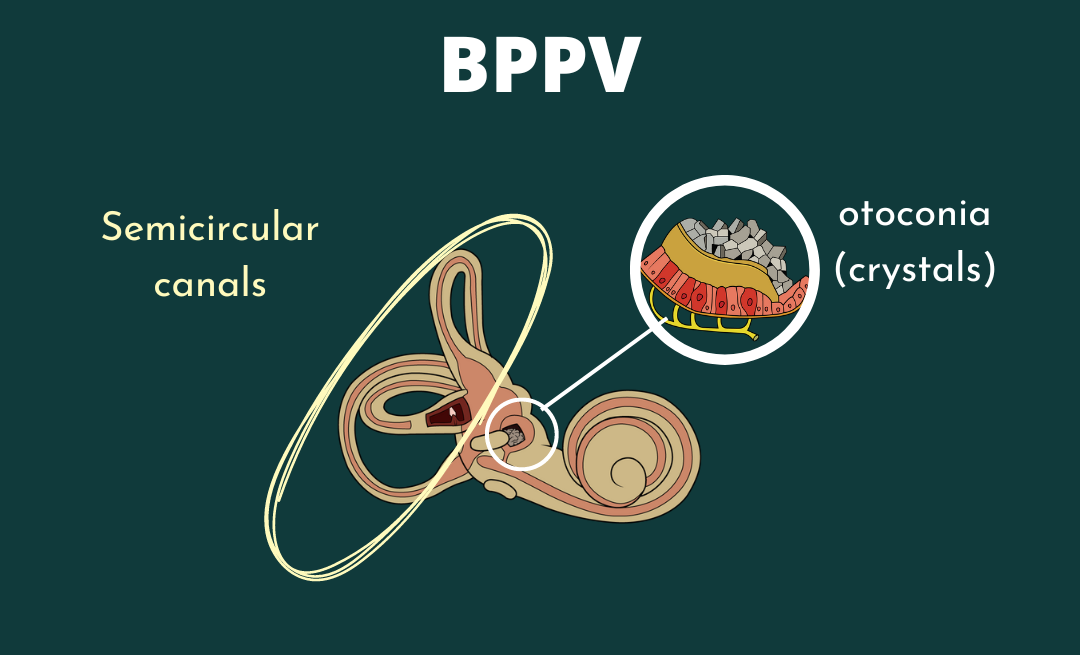
If the signal from our vestibular system isn’t sending or perceiving the correct information (BPPV, neuritis, VM etc), our brain starts to ignore what our vestibular system is saying and rely more on our visual system. Using only our eyes can result in busy environments making you feel dizzy or like you are moving when you really aren’t. The vestibular system isn’t being used in these situations to double check the information for our eyes. Things like busy areas like malls or restaurants, action scenes in movies, or first person video games can make your symptoms worse. Luckily, there are ways to work on reducing the reliance on your eyes and start using accurate vestibular information to feel better in busy environments.
How to promote visual vestibular integration.
Balance exercises that challenge vision help promote your vestibular and proprioceptive systems. With practice and gradual progression of these exercises, our brain starts to relearn how to listen to all 3 senses equally again. Consulting a trained and licensed vestibular therapist can help you safely progress these exercises and is strongly recommended. The goal is to start with sitting or standing balance exercises that make the visual and proprioceptive information hard to gather, so your brain has to rely on vestibular input to complete the exercise! This can be done in a variety of ways,a few ways a trained vestibular PT might accomplish this is:
- Eyes closed
- Eyes open with videos
- Firm surface
- Foam surface
- Standing feet apart or feet together.
There are many ways to tailor exercise individually and safely. Consult a professional to evaluate your specific needs and assist you in the safe progression based on your needs!
Want to learn more about visual vestibular integration, and other vestibular tools to get back to your daily life? Found out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Your hormones, dizziness and diet, with dietitian Susannah Juteau
Susannah is a registered dietician and headache nutritionist. Her focus is to address headache conditions like migraine and the use of diet to assist with lifestyle management and reduction of headaches or migraines! In group fit, Susannah sat down with Dr. Madison to discuss how food can impact hormones and how this can assist with migraines.
How can food impact hormones?
For a reminder on the many impacts of hormones on vestibular conditions, we have a blog post that reviews hormonal contributions to the vestibular system (click here) and how hormones change across the lifespan (click here).
Today the focus will be on estrogen and how diet can impact estrogen levels. Estrogen is an important hormone that can be a migraine trigger for some individuals 1,2,3. Rise and fall in estrogen levels throughout the female menstrual cycle can cause a flare up in headache, migraine or your vestibular condition. A change in estrogen levels is normal throughout this cycle, but diet can help avoid large increases in estrogen levels and sudden drops which can be beneficial to managing headache and migraine!1,2,3
Seed cycling is one way to use food and nutrition to assist with flare ups connected to your period. When Dr. Madison asked Susannah one thing that’s simple to try to help with estrogen levels, Susannah said eat more vegetables! Eating a plant based diet full of nutritious foods is a staple to health! We get so much dietary fiber, nutrients, micronutrients, and more from plants that cannot be found anywhere else in the world. Focus on eating a diverse number of foods throughout your whole life and each day for the best gut health! Susannah mentioned that these types of vegetables assist with breaking down excess estrogen and can help keep the fluctuation in estrogen levels in a more normal range to avoid big spikes and falls. This can help manage hormone related headaches.
What is the best Diet
There is no ONE diet or BEST option for dizziness and diet. Overall, avoiding overly processed foods and sticking to a whole foods diet is a good starting point while also reaching out to a registered dietician and nutritionist like Susannah Juteau for further guidance and education.
Dizziness and diet have a complex relationship between each other, and it’s important that we nourish our bodies with the right nutrients in order to get to a better place in our gut health, our brain health, and our vestibular health.
Keep in mind the benefits of a healthy diet for not only assisting with hormone fluctuations but giving your body the nutrients and fuel it needs for best function.
Vitamins and supplements can be helpful, but relying on only vitamins and supplements for nutrition can’t replace all the benefits from a healthy diet.
If you want more tips, check out what Susannah offers on her instagram sn services on her website!
Website: www.headachenutritionist.com/
Instagram: @headachenutritionist
If you’re interested in learning more about tests that could be helpful, other dietary tips to help with hormone and headache management, or catch the full interview with Susannah and a PDF of information, consider joining our vestibular community that includes dozens of premium content modules of information and resources and a great community to support you! Found out more at this link:
- SD;, S. (n.d.). Sex hormones and headache. Revue neurologique. Retrieved April 21, 2022, from https://pubmed.ncbi.nlm.nih.gov/11139745/
- World Migraine Summit. (2022). How Women’s Hormones Affect Migraine. Retrieved April 2022.
- Northrup, Christiane. (2015, May 29). Migraines. Christiane Northrup, M.D. Retrieved April 21, 2022, from https://www.drnorthrup.com/migraines/
Resources
Disclaimer
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Why do we get dizzy while driving?
Dizziness is a complex and frustrating symptom that often comes with driving. If you have ever been driving and had the overwhelming feeling that you need to pull over and stop, this might apply to you.
There are a few things that cause dizziness while driving. The first one is a binocular vision dysfunction like vertical heterophoria. This means your eyes are not aligned or they are struggling to work together as a team. I am not an eye specialist, but I can tell if eyes are having trouble teaming if you have difficulty with something like near-point convergence. This is the most common reason you will find on the internet for difficulty with dizziness while driving. However, there are other reasons you could be dizzy while driving, too.
Vestibular disorders and being dizzy while driving
People with vestibular disorders, like vestibular migraine, vestibular neuritis, meniere’s disease, and other frequently have difficulty with driving as well.
The dizziness while vestibular patients drive often presents similarly to those with binocular vision dysfunction. Most commonly, I see patients who describe their driving induced dizziness like they’re driving through a snow storm, like their visual system feels overwhelmed, or like they feel like the keep moving even when they’re stopped. This can cause severe anxiety associated with driving, a migraine attack while you’re in the car or when you get home, and more.
Another common complaint is getting feeling like you’re still moving even when you’ve stopped driving. If you pull into your driveway, or stop at a stop light and you feel like your body is still moving forward, you are absolutely not alone! I hear this constantly from my patients and clients. It’s a perception issue from your vestibular system and it can also be managed and treated.
If this sounds like you, there IS a solution. Vestibular Rehabilitation Therapy And Vestibular Group Fit™ are both excellent options for you.
Treating your driving related dizziness
Treating dizziness is best done with a holistic program that’s customized to you. You can customize it yourself, and you can use a qualified provider to help, as well! I recommend a combination of both.
The first step to treating driving related dizziness, is to determine WHY it’s happening. Many people have something called visual vertigo, and central peripheral visual integration issues. Visual vertigo is a common condition that comes from other vestibular disorders like vestibular neuritis, vestibular migraine, persistent postural perceptual dizziness, and other places. I often recommend finding the underlying condition, as well; but how to do that will be in another article.
After you figure out why it’s happening, which should be done with a qualified physical therapist, you can start retraining your brain and body to understand your surroundings.
Four steps to treating dizziness with driving
You and your physical therapist usually will take a few steps:
1. Watch a driving video taking up 90% of your visual field and reduce the anxiety that comes with driving.
2. Use Virtual Reality Goggles to make you feel as though your driving.
3. Slowly reintroduce you to driving in safe environments (empty parking lot, neighborhood, back roads, main roads)
4. Increase distance, speed, and more using your coping skills and managing your dizziness accurately.
Treat your dizziness with driving from home
Your dizziness can also be treated on your own if you’re the kind of person who thinks group coaching is a great fit for you! In Vestibular Group Fit™ we treat dizziness while driving in the Driving Module. This can be accessed only as a member of Vestibular Group Fit™. We go through why you may be dizzy with driving, exercises you can do while you’re driving, and how to return to driving safely. Click below to take the 3 Steps to Control your Dizziness & Vertigo MasterClass and start your healing journey!
What is sleep and why do we need it?
Sleep is defined as an altered state of consciousness. Research is ongoing to learn the importance of sleep. What we know so far is that sleep is an important part of our everyday life to help with healing and repair. Sleep gives our brain a chance to reset and allow our body to repair. Lack of sleep has been linked to other health issues such as anxiety and depression (Kim et. al).
There are two main types of sleep, light sleep and deep sleep. Light sleep is when you’re able to wake up more easily and spring into action if needed as a protective mechanism. Deep sleep can be broken down into slow wave and REM (rapid eye movement). Slow wave sleep is a time for your physical body to heal and be refreshed for the next day of movement. Deep sleep happens in the late hours of the night and into the early morning which is why having a consistent bedtime to capture these hours is important for healing both body and brain!
What does sleep have to do with my vestibular system?
Our vestibular system is connected to sleep in a number of ways. Thirty percent of those with vestibular disorders have reported an abnormal amount of time asleep and disrupted sleep patterns (Albathi).
When getting ready for sleep, our brain is listening to our vestibular, somatosensory and visual systems to know we are lying flat and aren’t moving so our brain knows our body is safe and ready to sleep. Those with vestibular conditions can have a harder time with sleep because their brain has a harder time getting this message that it’s time to rest.
Another connection of the vestibular system and sleep is when sleep levels increase, vestibular signals decrease. This is why drowsiness is commonly felt when motion sickness or vestibular systems worsen, and why sleep can help you feel better. In those without vestibular conditions, poor sleep showed slower reaction times and increased motion sensitivity. If you do have a vestibular condition, it is vital to get good and restful sleep for proper vestibular function.
Sleep and its healing properties can be extra vital for vestibular rehabilitation therapy. During REM, new connections are being made and strengthened in our brains and are important in forming new, positive connections with movement to help move with reduced or zero vestibular symptoms! Sleep is important for rehab and should be a part of your treatment and recovery.
Lastly, vestibular migraine has been shown to have a connection with sleep. Having good and consistent sleep is something we have discussed before as an important part of raising the migraine threshold. People with migraine may need more sleep than those without to help with raising their migraines threshold and vestibular recovery each day to reduce migraine attacks (Albathi).
Tips for better sleep
- Exercise regularly. Research shows that people who exercise regularly will have decreased risk of insomnia. This can be beneficial for anxiety, stress and general health too! (Banno)
- Keep a consistent sleep schedule. Even on weekends and vacations! Choose your favorite 7-8 hours; your brain LOVES a routine and LOVES a habit. And, a brain also managing a vestibular disorder loves ‘boring’. This means that you need to go to sleep and get up around the same time every single day.
- Sleep in a cool room. We need to drop our core body temperature by 2 degrees to fall asleep. Sleeping in a cool room, even if you’d like a big blanket, will help to optimize your sleep
- Get enough Vitamin D and B Vitamins. Not enough of either of these can reduce your ability to sleep, and can increase attacks.
- Try to avoid naps longer than 20 minutes. Napping longer than this in the day can make it harder to sleep at night.
- Establish a relaxing bedtime routine that you enjoy. Turn off the TV, stretch or do yoga, listen to a meditation, or something else relaxing. Remember to turn off all screens during this time
- If you don’t fall asleep within 30 minutes, get up out of bed. Get out of bed, and go to another room in your house. Sit on the couch, pull out a book or magazine, something analog is preferable and read for some time. DO not look at a screen, that will perpetuate the issue.
Other Resources
Dr. Stasha Gominac
Dr. Gominac spoke at the World Migraine Summit 2021. Dr. Gominac discusses the use of vitamins to help restore sleep quality and protect the body from migraines. Consider reaching out to learn more about her programming and consult your doctor if this would be right for you!
Louisa Nicola
Louisa Nicola is host of the podcast ‘The NeuroExperience Podcast’ and founder of NeuroAthletics. She has great FREE resources and content on her podcasts with interesting guests to listen to and learn from!
Want to learn more about sleep, the vestibular systems and ways to get better sleep? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources
Kim, Sung Kyun et al. “Relationship between sleep quality and dizziness.” PloS one vol. 13,3 e0192705. 7 Mar. 2018, doi:10.1371/journal.pone.0192705
Albathi, Monirah and Agrawal, Yuri. ‘Vestibular Vertigo Is Associated with Abnormal Sleep Duration’. 1 Jan. 2017 : 127 – 135.
Banno, Masahiro et al. “Exercise can improve sleep quality: a systematic review and meta-analysis.” PeerJ vol. 6 e5172. 11 Jul. 2018, doi:10.7717/peerj.5172
How to travel with dizziness
Living with a vestibular disorder is frustrating and can make you feel like you can’t do activities that once came naturally and easily to you. Traveling may be something that once came easily to you that now seems close to impossible. Busy visual environments, patterned carpets (hello, PDX), the anxiety about having a flare, and more can make it more anxiety provoking than fun.
However, I want you to know that it’s absolutely possible for you to travel with a vestibular disorder, you just may need to make a few adjustments!
10 tips to planning travel with a vestibular disorder
Just like with most things in the vestibular world, planning is going to be your friend here. Ask yourself a few questions before you decide what type of travel you’re going to do, and where you may want to go.
- Am I going somewhere new or familiar?
- Is my destination vestibular-friendly?
- Am I traveling alone or with a trusted person?
- What do I need to talk to my doctor about?
- What activities am I going to do when I get there?
- How can my vestibular physical therapist help me prepare for this trip?
- What can I pack to help me manage my symptoms?
- What’s my travel plan when I arrive?
- What mode of transportation am I taking?
- Does my diagnosis prevent my from traveling entirely?
When you have the answer to those questions, you can then consider how you can best support yourself throughout your trip. For instance, if you’re going somewhere like the Coast of California, you won’t have to really consider how the weather may affect you, but if you’re traveling to the East Coast then you may want to prepare to track the weather and treat accordingly.
Does my vestibular diagnosis prevent me from traveling?
In short, the answer to this question is no. However, there are a few factors to consider here. Ears ‘pop’ when you go up and down in elevation, whether it’s a fast elevator or a flight. If elevation changes bother you, then you should prepare for that. Otherwise something like driving or train travel is usually safe.
Safe to travel, in this case, means that you won’t do any extra harm to your vestibular disorder. It does not mean you won’t have a flare. This is why having the answer to the questions above and preparing accordingly is so important.
One last thing to note is 2 vestibular diagnoses that should be more wary of flight. The first is if you are undergoing surgery for superior canal dehiscence syndrome. In that case, you will want to wait the appropriate amount of time post-operatively before flying. Talk to your surgical team if you need to travel right after. The other diagnosis to be wary of it Perilymph Fistula. This diagnosis needs to be considered because sometimes pressure changes can indeed make the condition worse. As always, talk to your doctor.
Rapid elevation changes and your vestibular disorder
Traveling, whether it’s driving, flying, or otherwise, may have rapid elevation changes, this make your ear ‘pop’ and can cause symptoms or cause you to be uncomfortable. And, of course, that’s no fun, especially on vacation. So, how can we mitigate the affects of elevation changes on your vestibular disorder?
- Chew gum or eat while taking off and landing in an airplane
- Wear Ear Planes
- Avoid really high floors of a hotel with a fast elevator
- Avoid SCUBA diving and deep water diving
- Ask your doctor about taking a decongestant for the travel itself, which can help with your ear pressure
- Avoid unpressurized planes (hopper planes)
Planning travel around the weather and your vestibular disorder
Weather can be a really big factor for having attacks with a vestibular disorder. And in a world where we are doing everything in our power to avoid an attack, Mother Nature is not always in your favor. So, what can you do about it?
Track the weather with Accuweather:
- Google “Accuweather [insert city] migraine forecast”
- This tracks barometric changes and barometric pressure overall so you can track the weather and use your preventative treatment accordingly.
Consider where you’re headed. If you have a choice, maybe try somewhere that has fewer pressure fluctuations in general, and maybe somewhere with a temperate climate. This way you can enjoy the weather and your vacation without worrying about the weather. If you don’t have a choice, just pack according to the weather and what you’ll need – and I’m not just talking about clothes. You will also need to consider medications, preventive and rescue treatments, and more for your trip. And that’s okay, nothing a little extra planning can’t help!
Packing for travel with a vestibular disorder
So I know many people who overpack clothes, but not enough of us overpack essentials. Essentials for your day yo day life is what I am talking about here.
Medications
- Count out enough medications for the number of days you’re going, plus 2-3 extra days incase something happens
- Keep the medications, supplements, stimulation devices (like Cefaly and GammaCore, etc.) in your personal item so it’s easily accessible throughout the flight
- If you’re going to be changing time zones, be sure to ask your doctor/healthcare team about what
Nutrition & Hydration
Travel is really dehydrating in general. Bre sure you’re packing food and water with you on the place. You can’t bring liquids into the airport with you, so bring a water bottle with you instead and then fill it up when you get through TSA/security. If you’re driving, try and refill the bottle throughout the day, or bring more than one with you so you have enough to last you the whole trip . It’s really important that packing food that we are packing nutritious food. Road trips make us think (myself included) that we can eat junk and it will be fine. I’m not sure why we do this, but we do. So, instead of waiting for the gas station to stock up, pack food ahead of time and use the gas station for a treat if you want, instead of the other way around.
Tips for car travel
- Do a workout in the morning before the drive
- Get a good nights sleep before
- Eat a solid meal for breakfast before leaving
- Take a break every few hours to take a short walk
- Avoid high traffic hours
- Pack snacks and keep your blood sugar regulated
- Bring water and sip throughout the day
- Pack ginger chews for nausea
- Keep the windows cracked or the A/C on for cool air
- Stare at the horizon to keep your VOR steady
- Try to be the driver, if you’re safe to do so, rather than the passenger
Tips for plane travel
- Chew gum on the way up and down (or pop your ears otherwise)
- Walk while you’re in an airport for exercise and grounding
- Workout in the morning before leaving
- Get an excellent nights rest the night before
- Try to sleep on the plane, and bring a neck pillow
- Use grounding throughout the flight
- Pack a water bottle, I like this one because it has a straw which makes drinking in motion easier. Sip every 10-20 minutes, instead of chugging water
- Try and pick a seat over the planes wings so it’s not as turbulent
- Take extra magnesium with you if that’s a part of your treatment plan
- When you arrive, take a short walk to bring yourself back to baseline
- Try to arrive at night or in the evening so you can eat and head to bed – this will also help with the jetlag
How to manage visual stimuli with travel
Vision can feel like the issue when it comes to vestibular disorders, this is because your ears and your eyes are so connected.
So, instead of being miserable on your trip in stimulating visual environments, let’s talk about what you can do to help!
- Before your trip, ask your physical therapist to help you with visual vertigo exercises
- Join Vestibular Group Fit and use the Visual Vertigo Module to help you acclimate
- Wear tinted sunglasses when you’re outside (never inside) to help with light sensitivity
- Wear Avulux Glasses when you’re inside (and/or outside) to help with light sensitivity (use the code VERTIGODOC for a $25 discount)
Don’t Forget!!
As always, remind yourself that feeling dizzy, off, and generally uncomfortable after a long day of travel is actually really normal. Do the best you can to remind your body that you are safe, secure, and in a fun new place! Focus on having fun and less on what might happen during your trip.
Hormone levels change throughout the lifespan. Anecdotally, many of those with vestibular conditions appear to develop these conditions around these times of large hormonal changes. Let’s break down some of these milestones and how they relate to vestibular conditions.
Here is a quick breakdown of different time periods through a person’s life
- Prepubescent: infancy through puberty. 1-15 years old
- Reproductive age: after puberty, approx 15-40 years old
- Perimenopause: “around menopause” time before menopause when inter-menstrual irregularities and changes begin.
- Menopause: 12 months after final menstruation has occurred (1)
Prepuberty and Puberty & your Vestibular Disorder
One study has shown that in prepubescent males and females, the prevalence of migraine is equal at 4% occurrence. After puberty when a shift in hormones takes place and females have higher levels of estrogen, males with higher levels of testosterone, there becomes a dramatic change in migraine prevalence. After puberty, female prevalence in migraine is 18% and males is 6% (this is migraines in general and not vestibular migraines specifically). Part of what contributes to this change between males and females is attributed to the difference in estrogen levels. (2)
Pregnancy & Your Vestibular System
Typically, pregnancy has protective benefits from vestibular symptoms and migraines. The first trimester of pregnancy can be variable- some have worsening of migraines or new migraine symptoms such as an aura. Some experience migraines for the first time ever in the first trimester. In the second and third trimester there are higher estrogen levels which acts as a protection from migraines and most women typically experience improved symptoms. (3)
Talking to your doctor about supplements during and after pregnancy is important to keep you and your baby safe. Ask about B2, B6, folate, B12, vitamin D, magnesium, CoQ10, ginger, L-tryptophan and peppermint oil. (4)
Meniere’s disease may have a worsening of symptoms in the first trimester from fluid retention and reduced particles in the blood. This can impact how fluid is distributed at the semicircular canals and cause an attack. A diuretic or low salt diet may be recommended by your doctor to assist with reducing attacks during the first trimester. (5)
Post Partum & Your Vestibular System
Immediately after giving birth, estrogen levels drop. This can result in exacerbation of migraine or vestibular migraine symptoms. Another hormone that can be involved is prolactin which helps with milk production after giving birth. Prolactin is controlled by the hypothalamus in the brain. There are theories that hypothalamus involvement is linked to migraines. Not everyone feels a worsening of migraines when breastfeeding, 50% feel that breastfeeding has been protective against migraines. (3)
Other factors to consider are postpartum depression and new stresses of being a parent of a newborn that can make you migraine or vestibular symptoms worse. Look above in the pregnancy section to see what supplements to ask your doctor about. (6)
Perimenopause & Your Vestibular System
Perimenopause tends to be the time where people are noticing new or changing vestibular symptoms or conditions. Those who never had a vestibular migraine before will start having VM (people with and without a previous migraine history). (7) Some theories around migraine believe that estrogens’ impact on serotonin (a neurotransmitter responsible for pain and mood) can create a cascade leading to a migraine. Estrogen impacts serotonin, serotonin impacts the trigeminal nerve, trigeminal nerve has CGRP which has been shown to be involved with migraine (7). Perimenopause is a time where estrogen levels are more erratic which results in periods becoming further or closer together (and less predictable). This can be one factor contributing to the onset or worsening of vestibular migraine in perimenopause. Perimenopause also has more vasomotor symptoms (hot/cold flashes for example) which can impact symptoms. Risk of depression also increases at this time. This can have a widespread impact in other areas of your life, but can also play into worsening symptoms (8).
Menopause & Your Vestibular System
One full calendar year after one’s last period is considered menopause (1). Most with Meniere’s experience fewer attacks which can be theorized from fewer hormonal fluctuations (9). In this time of life, changes of BPPV increase and continue to increase as one ages. For migraines, there are fewer hormonal fluctuations but other contributing factors could continue to play a role in causing a migraine. It is important to continue to address these factors to optimize how you feel and gain control to manage your migraine (1).
Managing hormonal changes & Your Vestibular System
If HRT isn’t a great option for you, look at our previous article on Hormones and vestibular disorders to look at some other tips. Other things to keep in mind are:
- Address contributing factors (ex: neck or back pain)
- Exercise can assist with serotonin levels
- Certain foods can be helpful (think whole food/plant based food. Less processed foods)
Want to learn more about testosterone, oxytocin, progesterone and Q&A from other vestibular warriors?
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources:
- World Migraine Summit. (2022). How Women’s Hormones Affect Migraine. Retrieved April 2022.
- SD;, S. (n.d.). Sex hormones and headache. Revue neurologique. Retrieved April 21, 2022, from https://pubmed.ncbi.nlm.nih.gov/11139745/
- Sances G, Granella F, Nappi RE, Fignon A, Ghiotto N, Polatti F, Nappi G. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia. 2003 Apr;23(3):197-205. doi: 10.1046/j.1468-2982.2003.00480.x. PMID: 12662187.
- Beh, Shin C . Victory Over Vestibular Migraine: The ACTION Plan for Healing & Getting Your Life Back (p. 233). Beh Center for Vestibular & Migraine Disorders, PLLC. Kindle Edition.
- Andrews JC, Ator GA, Honrubia V. The Exacerbation of Symptoms in Meniere’s Disease During the Premenstrual Period. Arch Otolaryngol Head Neck Surg. 1992;118(1):74–78. doi:10.1001/archotol.1992.01880010078020
- Beh, Shin C . Victory Over Vestibular Migraine: The ACTION Plan for Healing & Getting Your Life Back (p. 229). Beh Center for Vestibular & Migraine Disorders, PLLC. Kindle Edition.
- Northrup, Christiane. (2015, May 29). Migraines. Christiane Northrup, M.D. Retrieved April 21, 2022, from https://www.drnorthrup.com/migraines/
- Migraine World summit. (2021). Overcoming Monthly Menstrual Migraine. Migraine World Summit. Retrieved 2022, from https://migraineworldsummit.com/talk/overcoming-monthly-menstrual-migraine/.
- NIH. (2016, April 25). Understanding how testosterone affects men. National Institutes of Health. Retrieved April 21, 2022, from https://www.nih.gov/newsevents/nih-research-matters/understanding-how-testosterone-affects-men
Hormones and Vestibular Conditions
Hormones are the chemical messengers for our body that travel through our bloodstream. They are in charge of so many of our bodily functions: hunger, emotions, growth and development, feeling ill etc. Research has shown a hormonal connection to the vestibular system and certain vestibular conditions. In this article we will look at estrogen’s and prolactin’s role in vestibular conditions. (1)
Estrogen is present in all humans but there are higher levels of estrogen in females. During childbearing years for females, estrogen levels change monthly throughout the menstrual cycle.
Estrogen levels drop 2 days before one’s period and right before ovulation; in between those drops there is a gradual rise in estrogen levels. The drop is estrogen during ovulation and before your period is when most people notice an increase in vestibular symptoms. (2)
Prolactin has over 300 roles but today we’re looking at its involvement with milk production and breastfeeding after childbirth. This hormone is controlled by the hypothalamus, and in some theories the hypothalamus plays a role in migraine. Based on the theories including the hypothalamus in migraine, prolactin could play a role in migraine in those who are breastfeeding. (3)
Meniere’s disease and Hormones
Common hormonal changes impacting Meniere’s disease are during the premenstrual phase of your period and pregnancy. Hormonal changes and fluid retention during these times can increase attacks. Fluid retention and hormonal changes can result in a change in fluid movement that can result in a Meniere’s attack. Research showed in one trial that those who had hormone therapy found some benefit in reducing the number of attacks. (4)
Acoustic neuroma and Hormones
Acoustic neuroma is a slow growing mass that impacts the vestibulocochlear nerve. This mass is typically benign and can cause imbalance, dizziness and hearing changes.
A study in mice showed increased growth of acoustic neuroma tissue. It appears that estrogen affects the pace of mass growth in acoustic neuroma. (5) Acoustic neuroma is also more common in women than in men, this may be in part due to higher estrogen levels in women, but more information and research is needed.
Vestibular migraine and Hormones
Migraine in general can be linked to hormonal fluctuations leading up to or at the start of one’s period (6,7). For vestibular migraine this may increase dizziness. The sudden drop in estrogen during menstruation and ovulation can cause an exacerbation of vestibular migraine. It’s been shown that migraineurs have a faster drop in estrogen than non migraineurs. (7,8). Another theory regarding migraine involves the relationship between estrogen and serotonin. Estrogen impacts serotonin, serotonin impacts the trigeminal nerve. The trigeminal nerve can cause migraines due to its release of CGRP. CGRP has been connect to migraine and the reduced ability to process CGRP, and anti-CGRP medicines were created to help treat migraines. (8)
Prolactin can also play a role in migraine. Both individuals with higher and lower levels of prolactin have been correlated with various types of migraines. Prolactin also has a connection to the trigeminal nerve and hypothalamus which have been theorized to have roles in migraines. (9). Prolactin has so many functions day to day so just a reminder that you don’t have to be breastfeeding for prolactin to have an influence on migraines. Breastfeeding is one of the many jobs prolactin is involved in, so if you’re breast feeding and notice changes, prolactin could be playing a role.
A side note: If you experience more headache symptoms with your migraine, research has shown addressing low testosterone (increase to higher levels within normal range) has been shown to reduce headache frequency. (10)
Managing hormonal changes
Hormone therapy is one way to address hormonal changes. This is a discussion to have with your doctor to see if this is a right fit for you. Hormone testing is generally not accurate because our hormone levels are always changing. Most hormone therapy involved dosing bioidentical hormones to help smooth out the fluctuations. This can be prescribed as a pill, patch, IUD or gel. (18/19). Some find hormone therapy helpful, others find that it makes symptoms worse, talk to your doctor about starting hormone therapy and give them updates on how your feeling so they can adjust your plan.
Other options to consider if hormone therapy isn’t for you are:
- Triptans: talk to your doctor if triptans could work for you and for your doctor to create and monitor your plan.
- Preventative medications: another great conversation for your doctor!
- Talk to your doctor about preventative supplements
- Magnesium
- Riboflavin (b2)
- Coq10
- Vitamin D
- Omega 3s
- GammaCore or Cefaly to assist with nerve stimulation for symptoms. (11)
Stay tuned for the breakdown of hormones throughout the different phases of life (puberty, pregnancy, post partum, peri/menopause) in our next article!
Do you want to learn more about how hormones can impact your vestibular condition?
Click here to Learn How to Manage Your Hormones & Vestibular Disorder
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Resources
- Kesserwani, H. (2021). Migraine triggers: An overview of the pharmacology, biochemistry, atmospherics, and their effects on Neural Networks. Cureus. https://doi.org/10.7759/cureus.14243
- Bb Natural Health. (2018, October 11). Cravings during your cycle. BB Natural Health. Retrieved April 21, 2022, from https://www.bbnaturalhealth.co.za/blogs/articles/91631363-cravings-during-your-cycle
- Tzabazis A, Kori S, Mechanic J, Miller J, Pascual C, Manering N, Carson D, Klukinov M, Spierings E, Jacobs D, Cuellar J, Frey WH 2nd, Hanson L, Angst M, Yeomans DC. Oxytocin and Migraine Headache. Headache. 2017 May;57 Suppl 2:64-75. doi: 10.1111/head.13082. PMID: 28485846.
- Andrews JC, Ator GA, Honrubia V. The Exacerbation of Symptoms in Meniere’s Disease During the Premenstrual Period. Arch Otolaryngol Head Neck Surg. 1992;118(1):74–78. doi:10.1001/archotol.1992.01880010078020
- Stidham KR, Roberson JB Jr. “Effects of Estrogen and Tamoxifen on Growth of Human Vestibular Schwannomas in the Nude Mouse.” Otolaryngology— Head and Neck Surgery, 120(2):262–264, 1999
- SD;, S. (n.d.). Sex hormones and headache. Revue neurologique. Retrieved April 21, 2022, from https://pubmed.ncbi.nlm.nih.gov/11139745/
- World Migraine Summit. (2022). How Women’s Hormones Affect Migraine. Retrieved April 2022.
- Northrup, Christiane. (2015, May 29). Migraines. Christiane Northrup, M.D. Retrieved April 21, 2022, from https://www.drnorthrup.com/migraines/
- Gazerani, P. (2021, September 24). A link between migraine and prolactin … – future-science.com. future-science.com. Retrieved April 22, 2022, from https://www.future-science.com/doi/10.2144/fsoa-2021-0047
- Watson, S. (2020, July 7). Low T and headaches: What’s the connection? Healthline. Retrieved April 21, 2022, from https://www.healthline.com/health/low-testosterone/headache
- Beh, Shin C . Victory Over Vestibular Migraine: The ACTION Plan for Healing & Getting Your Life Back (p. 229). Beh Center for Vestibular & Migraine Disorders, PLLC. Kindle Edition.
Food is medicine – nutrition and vestibular migraine with Kelli Yates, RDN
Food and diet can impact how we feel, and can play an important factor when it comes to the management of certain vestibular conditions. Your doctor may recommend certain dietary guidelines based on your vestibular condition and other factors (medications, other health conditions etc).
For vestibular migraine, certain foods can provoke your symptoms or trigger a migraine depending on how “full” your migraine threshold is on a given day. (click here to learn more about threshold/bucket theory and some additional information on migraine diets). If you’re not sure where to start with changing your diet, a registered dietitian or nutritionist can be a great resource and guidance in exploring how food can be medicine.
Kelli Yates, RDN, LD, CLT is a private practice registered dietitian and specializes in migraine and gut health. She became interested in this area while pursuing her own answers to help manage her migraine beyond medication. Kelli has self guided programs, 1 on 1 help with her personally, and great information that she shares with us all on her instagram (@the.migraine.dietitian).
Kelli sat down with Dr. Madison to discuss how food can impact our health, especially those with migraines of all types.
Kelli notes how food can be medicine as both a preventative and active treatment. In general, food is best used as a long term preventative. For migraine, this long term management of symptoms with food involves learning what foods provoke symptoms or trigger a migraine and in what quantity. Some foods may need to be avoided altogether and others you may be able to enjoy in moderation, it really depends on the person. An elimination diet can help reduce common food triggers for migraine and then you reintroduce foods to determine if they affect you.
Food can sometimes have an immediate effect. Peppermint and ginger can help with acute nausea and initial symptoms. Food schedules can also have a more immediate change on how you feel. Regular meal times/not skipping meals, or healthy snacks throughout the day can be a small change that could impact how you feel.
Here are some tips Keilli shared with us regarding diet and migraine:
- Reintroduce foods one at a time. There are many ways to introduce foods and a dietitian is a great resource to help tailor reintroduction to you!
- Low histamine diets are a temporary solution. If a low histamine diet helps, further care is needed to get to the root cause.
- Do what works best for you. Listen to your body on what feels good or bad. You know your body best. Keep that in mind before trying something that is suggested you try or you were told worked for someone else.
If you want to hear more from Kelli, follower her on instagram @the.migraine.dietitian or go to her website https://kelliyatesnutrition.com/
Kelli talks more about reintroducing foods, why low histamine diets are only temporary solutions, probiotics, gut health testing and anxiety around food in her talk with Dr. Madison.
Do you want to learn how to manage your vestibular disorder holistically, through diet and more?
Click here to Manage your Vestibular Disorder Better
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.