Persistent Postural Perceptual Dizziness (PPPD) is chronic, long lasting, dizziness that is non-vertiginous and fluctuating in nature (1). PPPD is a relatively new diagnosis; the diagnostic criteria were created in 2014 and for that reason many providers don’t know about the condition or the criteria (1). PPPD has signs and symptoms that present like many other vestibular diagnoses including vestibular migraine, vestibular neuritis, or anxiety related dizziness making it even more difficult to diagnose. Prior to being titled Persistent Postural Perceptual Dizziness, PPPD was referred to names including: phobic postural vertigo (PPV), space-motion discomfort (SMD), visual vertigo (VV) and chronic subjective dizziness (CSD) (2). The criteria of these have now been combined to form Persistent Postural Perceptual Dizziness and has specific criteria designed to provide an exact diagnosis (3).
It is not always possible to determine an exact cause of PPPD, however it rarely comes on slowly. Your balance system, which consists of three systems working together to keep you stable, is in a state of disequilibrium when you have PPPD. Instead of the three systems seamlessly working together for stability, your body has difficulty processing the information passed between them, making your brain feel like you may fall over at any moment. This feeling places your body on high falls risk alert, and the more you worry, the more anxious you may become. This anxiety causes an increase in dizziness, which then increases anxiety. This is a vicious anxiety cycle. All of this can be treated in vestibular physical therapy with your team of healthcare providers.
Symptoms & Diagnosis
Symptoms of Persistent Postural Perceptual Dizziness vary widely from one individual to the next. The symptoms have an inciting event that caused the original onset of symptoms, and can be either vertiginous or non-vertiginous, even if you can’t remember when it occurred. This event can be any event that caused dizziness, either physical or psychological, and includes: (2)
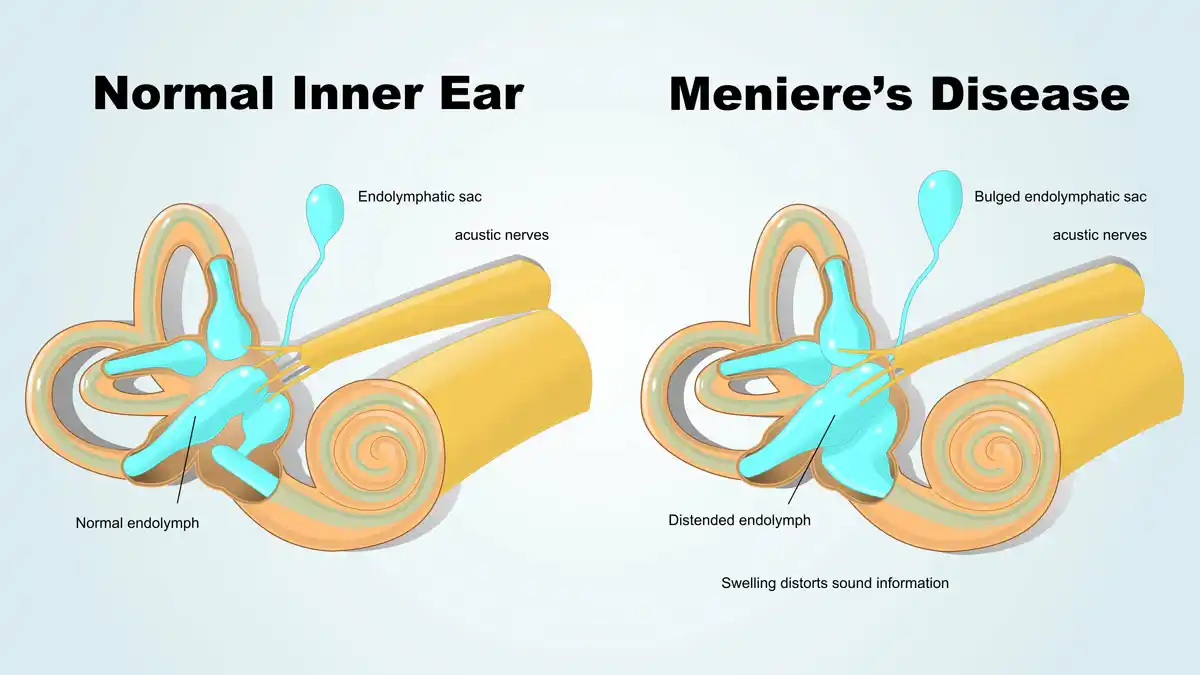
- Meniere’s Disease
- Vestibular Neuritis
- Vestibular Labyrinthitis
- Benign Paroxysmal Positional Vertigo (BPPV)
- Vestibular Migraine
- Panic or Anxiety Attack
- Concussion or Mild Traumatic Brain Injury
Any of these, or other vestibular conditions, can be the cause of PPPD. There many symptoms related to Persistent Postural Perceptual Dizziness, including:
- Rocking or swaying when you are being still
- Unsteadiness
- Lightheadedness
- Feeling spaced-out or dissociated
- Anxiety or fear
Symptoms are exacerbated with:
- Sitting or standing (upright posture)
- Seeing movement (phone scrolling, traffic passing by, watching TV)
- Looking at complex patterns (busy background or carpets)
- Walking
- Riding in a car
- Passive and/or active motion
Other symptoms frequently reported are:
- Neck pain or tightness
- Fatigue
- Fear of falling, imbalance
- Problems or changes with how you walk
- Fear avoidance (avoiding stimulating activities you would normally participate in)
These symptoms are both directly and indirectly related to your experience with Persistent Postural Perceptual Dizziness. Your healthcare providers, especially your physical therapist, should be made aware of the symptoms you are experiencing. The more information that they have, the better your provider will be able to assist you in a diagnosis recovery.
Because PPPD is such a new diagnosis, the criteria is widely unknown to many providers. However, we are all able to access them, and they can be found below. If you fit this criteria, vestibular therapy will be an avenue to help your recovery. The following are the official diagnostic criteria for Persistent Postural Perceptual Dizziness, all 5 must be met (A-E) to fit the diagnosis: (3)
- A. One or more symptoms of dizziness, unsteadiness, or non-spinning vertigo are present on most days for 3 months or more.
- 1. Symptoms last for prolonged (hours-long) periods of time, but may wax and wane in severity.
- 2. Symptoms need not be present continuously throughout the entire day.
- B. Persistent symptoms occur without specific provocation, but are exacerbated by three factors:
- 1. Upright posture,
- 2. Active or passive motion without regard to direction or position, and
- 3. Exposure to moving visual stimuli or complex visual patterns.
- C. The disorder is precipitated by conditions that cause vertigo, unsteadiness, dizziness, or problems with balance including acute, episodic, or chronic vestibular syndromes, other neurologic or medical illnesses, or psychological distress.
- 1. When the precipitant is an acute or episodic condition, symptoms settle into the pattern of criterion A as the precipitant resolves, but they may occur intermittently at first, and then consolidate into a persistent course.
- 2. When the precipitant is a chronic syndrome, symptoms may develop slowly at first and worsen gradually.
- D. Symptoms cause significant distress or functional impairment.
- E. Symptoms are not better accounted for by another disease or disorder.
Treatment
Vestibular Rehabilitation Therapy, or VRT, is effective in treating PPPD in conjunction with Cognitive Behavioral Therapy, education, and potentially some medications. Vestibular Rehabilitation Therapy is effective in habituating and adjusting your brain through neuroplasticity, or the ability for your brain to change and mold to its environment. Although there have been no randomized control trials at this point, clinical experience and reports show that 3-6 months of VRT is often very effective in treating your symptoms (1).
Additionally, Cognitive Behavioral Therapy (CBT) can be effective for some individuals who have new PPPD symptoms, but is less effective for those who have had symptoms for a long time. If you begin Cognitive Behavioral Therapy within 8 weeks of symptom onset, the results from CBT are lasting and effective (1).
Medications can also be effective in treating PPPD, some physicians prescribe SSRI’s and SRNI’s to help with symptoms of anxiety and dizziness. It has been found that symptoms were reduced by at least half in 60-70% of patients who were on one medication or the other for 8-12 weeks. Patients who had lasting effects were on the treatment for at least one year. Medications such as Benzodiazepines and vestibular suppressants, most commonly Meclizine, were found ineffective in treating PPPD symptoms (1).
There are many different treatments for PPPD, however treating the symptoms and the root cause simultaneously will have the longest lasting effect. Combining VRT, CBT, and medication will help you begin to feel like yourself as quickly as possible.
Physical Therapy
The main and most effective form of treatment for PPPD is Vestibular Rehabilitation Therapy. VRT is prescribed by your physical therapist to slowly adjust your tolerance to stimuli that bother you. For some, a stimulus could be patterned carpets and for others it could be head motion. Whatever the stimuli, VRT can help you. Your physical therapist will adjust the dosage of irritating stimuli to your symptoms using the 15 minute rule. In physical therapy your PT will grade the amount of a stimulus you can tolerate and dose your exercises accordingly. Do not attempt to dose PT yourself as I find patients often overstimulate themselves leading to a big flare up.
Sources:
(1) VEDA. (2020, May 21). Persistent Postural-Perceptual Dizziness. Retrieved September 07, 2020, from https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/persistent-postural-perceptual-dizziness/
(2) Balance and Dizziness. (2019, September). Persistent Postural-Perceptual Dizziness (PPPD). Retrieved September 08, 2020, from https://balanceanddizziness.org/disorders/vestibular-disorders/pppd/
(3) Staab, J. P., Eckhardt-Henn, A., Horii, A., Jacob, R., Strupp, M., Brandt, T., & Bronstein, A. (2017, January 01). Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Bárány Society. Retrieved September 09, 2020, from https://content.iospress.com/articles/journal-of-vestibular-research/ves622