Dizziness triggers: threshold theory and 10 contributors to dizziness
Many are on the hunt for dizziness triggers. “What is the one or two things that make my dizziness worse”. “If I just figured out my trigger I can get rid of it and not be dizzy anymore”. The many variables in day to day life, both within and outside our own control, makes this a futile effort. This leads to feeling overwhelmed, hopeless, frustrated, and depleted. This article will discuss a different approach known as threshold or bucket theory as well as considerations of what may contribute to one’s threshold. We’ll also cover ways to track this and create a bigger threshold for long term growth and management.
What is threshold (bucket) theory? Why is this better than finding specific dizziness triggers?
Finding specific dizziness triggers or the root cause to dizziness sounds great in theory but much harder in practice. Each day is different, making this hard to track. There might be areas that might contribute to dizziness but is outside anyone’s control (weather, infection, allergies) so then what?
Threshold or Bucket Theory helps account for the variability of life, things within our control and outside our control, and why it’s rarely just one thing. Think of a bucket, and dizziness triggers fill up the bucket. Different things may fill up the bucket more or less on different days. On better days we might have a bigger bucket, on less ideal days the bucket is smaller. When the bucket starts to reach full capacity or even starts to overflow, symptoms are heightened or even a full on attack.
Looking at what may contribute to ones bucket can help strategize and know what days may be more challenging and more support is needed, see what is within our own control to be modified, finding grace for things outside ones control, and working on growing a bigger bucket.

Contributors to threshold (or possible dizziness triggers depending on the day)
The picture above illustrates threshold theory and common “dizziness triggers” or contributors to ones threshold. This better shows how it’s rarely one thing that sets off a dizziness flare or attack and more likely a combination of factors, including a lower threshold/smaller bucket. Listed below are common contributors, and we’ll go into a bit more detail in the next section.
- Stress
- Poor Sleep
- Poor Hydration
- Hormones
- Weather Changes
- Illness/Sickness
- Dizzy Anxious Cycle
- Environment
- Seasonal Allergies
- Muscle tightness/Lack of MovementLet’s dive deeper into each of these topics below!
- Stress: High levels of stress can exacerbate vestibular symptoms by triggering physiological responses like the fight or flight response. Stress can tie into the dizzy anxious cycle but can be it’s own separate contributor as well. Chronic stress can lower ones threshold can lead to other health impacts such as poor sleep, muscle tension, headaches, high blood pressure and more.
2. Poor Sleep: Inadequate or poor-quality sleep can disrupt the body’s natural rhythms and impair cognitive function and processes that help with memory and learning. Learning is an area that’s important when healing and recovering from vestibular conditions as part of positive neuroplasticity. Learning and brain function help with reweighing of the sensory systems (why Vestibular therapy works!) Sleep deprivation can lower ones threshold by making it harder for the brain to carryout tasks. With a vestibular condition, the brain is working harder to determine spatial orientation and movements, and trying to determine the correct response. When functions require more resources, sleep is important to optimize function.
3. Poor Hydration: Dehydration can disrupt the balance of fluids and electrolytes in the body, affecting blood pressure and circulation. This may be important in certain populations such as those with POTs (Postural Orthostatic Tachycardia Syndrome). Being properly hydrated is again important to best support the body for healing and recovery.
4. Hormones: Fluctuations in hormone levels, such as those experienced during menstruation, pregnancy, or menopause, can influence vestibular function and trigger dizziness. There are some blog posts that go into more detail on the website. But there’s some amazing in depth information and discussions for Vestibular Group Fit Members.
5.Weather changes: Variations in barometric pressure, temperature, and humidity can contribute to ones threshold. Think of weather as a possible stressor to the body. Sudden changes in weather conditions may lower the threshold for dizziness and vertigo, especially for individuals with sensitivity to atmospheric pressure changes. The weatherx app and ear plugs can better assist tracking possible connections to barometric pressure shifts, and weather x ear plugs to assist in minimizing the impact of the weather.
6. Illness/Sickness: Viral infections, bacterial illnesses, and other health conditions can add stress to the body. As the body is fighting off an infection, energy and resources are being diverted to fight off an illness. Illness-related symptoms may lower the threshold for experiencing vestibular symptoms, particularly during periods of acute illness or recovery.
7. Dizzy-Anxious cycle: The relationship between dizziness and anxiety can create a vicious cycle where dizziness triggers anxiety, and anxiety exacerbates dizziness symptoms. This cycle can quickly fill ones threshold. This cycle can be broken, and why mindfulness and mindset work is so so important. Consider a professional to assist with tools and coping strategies. A whole section on medications, breathwork, and tools are in Vestibular Group Fit for members to explore.
8. Environment: Environmental factors such as noise, lighting, and visual stimuli can worsen dizziness. Certain environments, such as crowded or visually stimulating spaces, may lower ones threshold as well if visual vertigo or motion sensitivity is part of ones vestibular condition (hint: it is for many).
9. Seasonal allergies: Allergic reactions to pollen, dust, or other environmental allergens can exacerbate inflammation and congestion in the sinuses and even feel like plugged ears. Seasonal allergies may lower the threshold for experiencing dizziness and vertigo, especially during peak allergy seasons, everyone responds to allergies different, but springtime can be tough for vestibular warriors between weather shifts and pollen counts.
10. Muscle tightness/Lack of movement: Muscle tightness, especially in the might back, upper trap and neck region can impact migraine conditions and dizziness. Muscle tightness and resulting pain or a state of discomfort can make other symptoms worse as well. The body likes to move, and having tight, stiff, painful muscles or a fear of movement from dizziness and unsteadiness can become a vicious cycle.
How to track dizziness triggers or your threshold contributors
Using apps like Migraine Buddy or keeping a symptom journal can be valuable tools for tracking possible dizziness triggers in individuals with vestibular disorders. However, it’s important to approach symptom tracking mindfully to avoid hyperfocus, which can exacerbate symptoms and diminish quality of life. Rather than constantly monitoring, it’s recommended to track symptoms after noticing an increase or flare in dizziness.
Record information from the past 1-2 days, things like:
- hormonal fluctuations.
- stress levels
- weather
- allergies
- meals (skipped meals, different meal times, missed a bedtime snack, less nutrient dense meal etc)
- sleep
If experiencing increased symptoms or a flare, consider tracking symptoms leading up to the event, any medications taken, and strategies employed for relief. This can help identify patterns or prodromal signs preceding an attack and evaluate the effectiveness of medications or interventions. Remember, the goal is not to obsessively monitor every moment, but to gather insightful data that can inform targeted interventions and improve symptom management over time.
How to get a bigger threshold
Growing a larger threshold over time to better manage vestibular disorder symptoms involves a holistic approach that encompasses various aspects of health and well-being. Luckily, some of these are little to no cost, no doctors prescription needed. Building a bigger bucket does require consistent routine changes. Start small start slow. Build up a new routine one thing at a time, then add another. Check out a podcast on this here.
Just a reminder as well, certain factors like allergies, weather fluctuations, or illness may be beyond our control. Focusing on strategies within our control can help grow a larger threshold over time, allowing us to better absorb dizziness triggers we cannot control. There are some tools to try such as Weather X ear plugs before barometric pressure shift, allergy medication or natural nasal spray, measures to reduce risk of illness during cold and flu season. These may be good and useful tools to implement based on the situation.
Ways to grow a bigger bucket:
- Consistent, high-quality sleep is fundamental, as it supports overall health and resilience to stress.
- Regular movement, tailored to individual capabilities, promotes physical strength and balance, while staying adequately hydrated ensures optimal functioning of bodily systems.
- Engaging in mindset work and stress management techniques can help cultivate resilience and reduce the impact of stressors on symptoms.
- Environmental changes/workplace accomodations such as blue light glasses like avulux, blue light filters for computer use like iris tech, light covers for overhead fluorescent lighting, loop ear plugs etc.
- Seeking assistance from healthcare providers and building a supportive provider team can offer valuable guidance and resources for symptom management.

Living with a vestibular disorder requires patience, resilience, and a proactive approach to managing triggers and symptoms. By incorporating lifestyle modifications, stress management techniques, and awareness of your personal threshold, you can take control of your condition and improve your overall well-being. Remember, you’re not alone in this journey, and seeking support from healthcare professionals and fellow individuals living with vestibular disorders can provide valuable guidance and encouragement. Together, we can navigate the challenges of dizziness and find moments of stability and balance in our lives.
Disclaimer
Want to learn more about threshold contributors, tools to manage contributors, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
7 Ways to find support for vestibular conditions
Having support for vestibular conditions in various aspects of life are essential for navigating this challenging journey. Vestibular conditions truly take a village of friends, family, providers, and professionals to help along the path to confident management. In this blog post, we’ll explore various avenues for seeking support and connecting with others who understand what you’re going through.
7 areas to find support for vestibular conditions
- Support Groups
- Counseling
- Return to Work Accommodations
- Medical Intervention
- Holistic Intervention
- Friends and Family
- Success Stories
1. Support for vestibular conditions: Support groups
In today’s digital age, online communities have become invaluable sources of support and solidarity. Platforms like Facebook groups, Reddit communities, and online forums host discussions where individuals share experiences, coping strategies, and encouragement. Joining these groups can provide a sense of belonging and reassurance that you’re not alone in your journey. There are some great vestibular warriors and providers that help host local and online support groups. Here’s some resources on finding one to join.
2. Support for vestibular conditions:
Counseling
Living with a vestibular condition can take a toll on your mental health, leading to feelings of anxiety, depression, or isolation. Seeking counseling or therapy can be immensely beneficial in navigating these emotional challenges. A professional can help provide a safe space to vent and work through challenging emotions and grieving that is so normal to arise. It can be hard to find a professional that knows both counseling and vestibular conditions. One provider that does is Dr. Emily Kostelnik (The Vestibular Psychologist) Who is a licensed clinical health psychologist and fellow vestibular warrior. Her and her team of mindset coaches are great to work with. Other options for support for vestibular conditions include a therapist that has background in chronic pain. Chronic pain can have similar overlap to chronic dizziness. Finding a provider can be done through different databases. Feel free to check out here & here. It can take some time to find a counselor that really clicks; it’s okay to switch therapists!
3. Support for vestibular conditions: Return to work accommodations
Vestibular conditions make most, if not all, jobs challenging to complete. This does not mean returning to the same job can never happen. People have returned to work. This can look like a gradual return to work program and/or requesting reasonable accommodations to support job tasks. Going part time and building up hours, blocking off certain parts of the day to space out challenging tasks, requesting an office location that is quiet, remote work etc. More on this in a blog post here. The Job Accommodation Network is a great resource as well to learn what accommodations are common with dizziness, and prompts to help determine what may be requested based on specific job tasks. Return to work can include a combination of other interventions as well as modifications to best give support for vestibular conditions.
4. Support for Vestibular Conditions: Medical intervention
Navigating the medical side of vestibular conditions can be murky. Understanding how the vestibular system works (video here). Can turn fear into empowerment. Understanding which providers can be helpful or finding ones to team up and help create a management plan can help give the body the support needed to recover. Navigating specialists, tests, and various treatment routes can be hard to do alone. Having resources and community from others who have experienced this can help.
5. Support for Vestibular Conditions: Holistic intervention
Holistic work has its own seat at the table. Meditation, mindfulness, tai chi, yoga, herbs, supplements, guided visualization are different ways a holistic approach can be incorporated. Finding calm and safety is important for taming the dizzy anxious cycle and rewiring movements to mean safety. Finding self compassion and acceptance is huge here as well.
6. Support for Vestibular Conditions: Friends and family
Finally, don’t underestimate the power of building a personal support network comprised of friends, family, and loved ones. Communicate openly with those close to you about your condition, how it impacts your life, and what support you need. Their understanding and empathy can provide a strong foundation of support as you navigate the ups and downs of living with a vestibular disorder. This can be challenging and something talked about in detail within small group coaching and Vestibular Group Fit. Check out this episode that discusses dating, or this blog.
7. Support for vestibular conditions: Success stories
Knowing you aren’t alone is a huge weight off ones shoulders. But what about next steps? Or hope for the future? Hearing others journeys and successes is an uplifting reminder that you aren’t alone and it does get better. Here are some written options, and more with audio at Grounded: The vestibular podcast
Vestibular Group Fit
All this and more can be found in Vestibular Group Fit. This low cost monthly subscription has education, community, support and guidance to answer your questions and find your path to healing and management. Learn about the ‘why’ here.

Disclaimer
Want to learn more about strategies, information, tools and support for vestibular conditions? Get vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Best steps to Treat MDDS (Mal de Debarquement Syndrome)
Learn about what MDDS is, how it can be treated, and other resources to learn more about MDDS management.
Diagnosis criteria for Mal de Debarquement Syndrome
Criteria for the diagnosis of Mal de Débarquement syndrome
- Non-spinning vertigo characterized by an oscillatory perception (rocking, bobbing, or
swaying) present continuously or for most of the day. - Onset occurs within 48 hours after the end of exposure to passive motion.
- Symptoms temporarily reduce with exposure to passive motion.
- Symptoms continue for >48 hours. (More on this in the next section)
- Symptoms not better accounted for by another disease or disorder.
MDDS diagnostic criteria has changed slightly to include a spectrum of time someone has been experiencing symptoms. This has been designed to help those get a diagnosis and begin treatment sooner which is a great addition. Here they are:
- MdDS in evolution: symptoms are ongoing but the observation period has been less
than 1 month - Transient MdDS: symptoms resolve at or before 1 month and the observation period
extends at least to the resolution point - Persistent MdDS: symptoms last for more than 1 month
3PD vs MDDS: what are the differences?
When searching for answers and finding a diagnosis, it can be tough to know which description fits best. You can also have more than one vestibular condition to make diagnosis more challenging. Dr. Madison talks with Vestibular Group fit Members the differences between Vestibular Migraine, PPPD, and MDDS as well as treatment considerations if you have a combination of diagnoses.
In this blog we’ll briefly talk about some differences between 3PD (persistent postural perceptual disorder) and MDDS
3PD
- People typically feel worse in car
- Will typically feel worse with walking/movement
- additional 3PD criteria can be found in this blog post here.
MDDS
- People usually feel better in car
- Will tend to feel worse with walking
Non-motion triggered Mal de Debarquement Syndrome
If you’re searching for answers, you might come across non-motion triggered MDDS. This area of vestibular research and classification is still up for debate. Some think this is a different form of chronic dizziness, or vestibular migraine, or something else. Time will tell where this ends up!
MDDS treatment: Dai protocol
A very popular protocol for MDDS treatment is the Dai protocol. A 2018 research study by Dai et al show that 75% of those undergoing treatment had significant improvement when followed for 1 year. This protocol involves a few important tests and equipment to follow and is best to be done with a provider knowledgeable in this protocol. If you’re in a place where a provider isn’t familiar, they can read research and implement the protocol with you.
More information on the Dai protocol can be found here.
A great treatment tool for MDDS or other visual vertigo can be found here through 360 Neuro Health. Talk to your provider before using to find the best dosage and progressions.
Mal de Debarquement Syndrome treatment continued
There are more treatment considerations than the Dai protocol. Medications such as SNRIs/SSRIs and benzodiazepines have been shown to be a beneficial part of treatment for some.
Other factors to consider as part of treatment include:
- sleep
- diet
- exercise
- stress management
- vestibular exercises/VRT
- mindset
- neuromodulation
Dr. Shin Beh goes into detail on MDDS and treatment in his book Disembark, check it out here as well as other great books Dr. Beh has written.
Disclaimer
Interested in learning more? Check out this other blog post on Mal de Debarquement Syndrome
here.
Want to learn more about MDDS, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Learn tips for dating with a vestibular disorder. We cover dating, relationships and intimacy with Dateability cofounder Jacqueline Child.
Dateability: A Dating app for those with disabilities and chronic illnesses.
Dating with a vestibular disorder can be challenging or intimidating to begin after a receiving a vestibular diagnosis. Jacqueline Child is a co-founder of Dateability and talks with Dr. Madison oak about dating and intimacy with chronic illness and disabilities. Jacqueline encountered ableism on other dating apps, and experiences impacting her self esteem. In october 2021 after a feed tube surgery, Jacqueline expressed her wish for a dating app tailored to people like herself. Jacqueline’s sister proposed they make this wish a reality. Dateability aims to foster understanding, compassion and connection to provide a safe space where chronic illness is not a deterrent to finding meaningful connections and love. Learn more about this app here.

5 Suggestions when dating with a vestibular disorder
1.You’re more than your vestibular condition! Talk about other interests, projects or hobbies you have going on or hope to start!
2. Explaining your vestibular condition can be short and simple at first. Jacqueline compares it to how you’d explain your condition to a child. Remember, you’ve learned so much about your condition, that it can be overwhelming to someone that is learning. This can vary based on their exposure to the medical field as well (vocabulary and health literacy etc). Keep it easy, if they have follow up questions and you want to answer them, go for it!
3.If there’s an activity that doesn’t work great for you, let your needs known and suggest an alternative activity. When dating with a vestibular disorder, certain activities might not be the best for you. Instead of saying no to their suggestion, feel free to let me know that won’t work for you and suggest an alternative activity that works for you. For example swap out a bike ride for a picnic in a park, or maybe a tram bike that moves slower and multiple people steer and peddle.
4.Be honest about your needs early on. You don’t have to list them all out day 1, but when something comes up, mention the relevant information or accommodations needed. For example, if someone suggests a movie and the time is late. Casually mention that staying up late isn’t great for you, and see if the there’s an earlier showing.
5.Communication is key when dating with a vestibular disorder, and discussing your vestibular condition is a very vulnerable thing to do. Practice can help, whether it be with close friends and family, or going on some dates just to practice how you share your story with someone new.

Tips for Discussing Chronic illness in Dating or with your current partner
- Communication is so important. Be honest about how you’re feeling, and limitations.
- not communicating your feelings and needs is unfair to yourself and your partner. Expressing your feelings and needs is the best way for others to understand what’s going on. Assuming others can read your mind can make everyone frustrated.
- hiding symptoms and pushing beyond your limits to appease others ends up backfiring in the end
- Have a codeword or phrase to convey you’re not feeling well. It lets other know what you’re feeling without having to put it into so many words.
- Longer conversations and explanations might not be necessary at first. But can be beneficial to have eventually to ensure understanding, trust, and building a deeper connection.

Navigating intimacy with vestibular disorders
Intimacy and sex is an area that is important to address when it comes to dating with a vestibular condition and relationships. This part of romantic relationships can be a source of apprehension when dating or looking for a long-term partner. Communication here is so important (sensing a theme about communication?).
Having a conversation outside of intimacy and sex can help. Knowing modifications or positions that are best, or how to handle situations when a pause is needed beforehand will help in the moment to do what’s best for your body. This may feel uncomfortable or awkward, but communication is about trust, and knowing your partner cares about you to support you and want what’s best for you in all aspects of life.
Disclaimer
Want to learn more about dating, relationships, other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Learn more about gaining self compassion with your vestibular condition and how to adapt mindfulness practices to best suite your needs. Fellow Vestibular Group Fit member Melina is a certified mindfulness instructor and shares her expertise on self compassion and mindfulness but with a chronic illness and vestibular focus.
Meet Melina
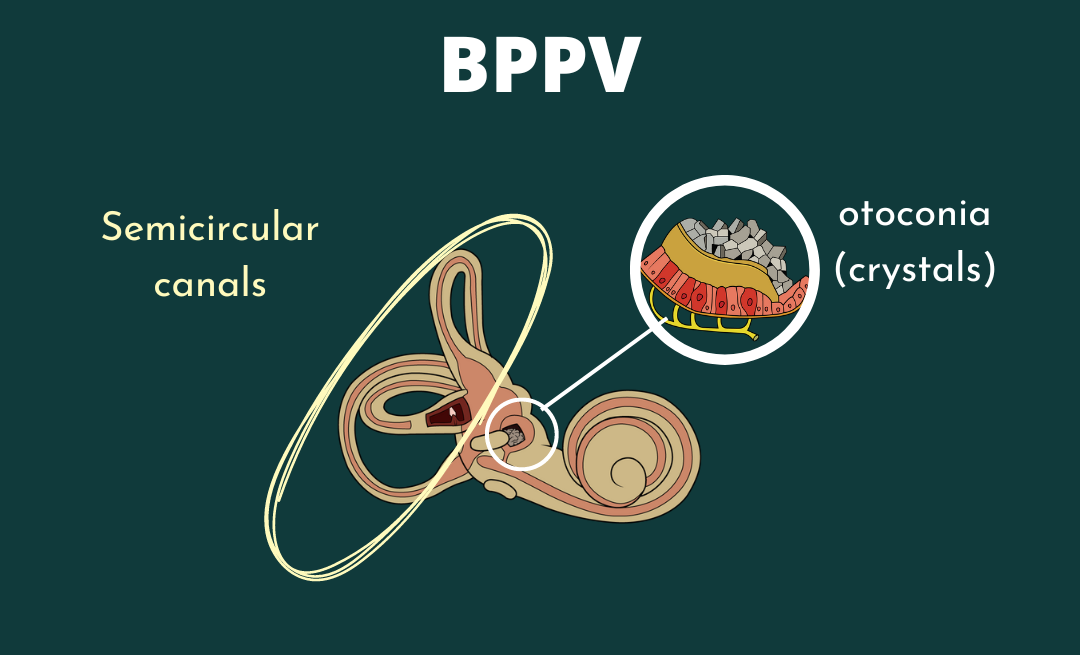
Melina is a certified mindfulness educator who offers classes in her community and as a professor at the University of Rochester. She is also a member of Vestibular Group Fit. Her research and teaching interests include music and the body, the history of somatic practice, and embodied pedagogy. Because she lives with recurrent BPPV and vestibular migraine, much of her meditation teaching focuses on mindfulness for chronic illness and pain.
What is self compassion
Self compassion can feel like this ellusive thing everyone talks about but doesn’t really understand. Melina offers a great definition. Self compassion is about acknowledging struggles, offering ourselves comfort, and extending kindness to ourselves and others facing a similar experience. You are not alone, others have felt exactly what you are feeling now, and that shared human experience unites us to humanity.
Basically, self compassion is treating ourselves the way we would a close friend who is struggling. We want to extend ourselves the same acceptance we have for our close friends or family. We embrace them for who they are, imperfections and challenges and all. Self compassion is doing the same for yourself.
Self compassion has positive benefits, including calming our nervous system, and can be an important tool in healing and growth. Self compassion can enhance other mindset work you’re already doing for continued growth and impact. Using self compassion with a vestibular condition can assist in weathering flares or daily challenges while becoming resilient for future challenges.
How to adapt mindfulness practices for you
1.Have a gentle approach. Don’t force changes in thought. Allow yourself to be present in your discomfort. Respond with kindness and allow your body to focus on other thoughts, feelings and sensations as one retreats and another announces its presence.
2. There is no set guidelines you must follow. Pick and choose what you like. There are different anchors available to work on being in the present. A popular anchor is focusing on your breathing. Try the “choose your own anchor” practice. For this practice, be aware of your vestibular symptoms, and in addition to ours symptoms, focus on something pleasant or neutral. This acknowledges your challenges while finding moments of peace and balance within.
Not sure about positive or neutral areas to focus on? Visit the post on mindfulness and critical thinking that dives into this more here.
3. Create a mindful and safe space. This can be in any position you find comfortable, finding anchors that best fit to your style and needs, picking and choosing different practice aspects that you enjoy.
Melina also recorded three tracks to work on self compassion, mindfulness, and with a vestibular focus. These are available to vestibular group fit members, if you’re interested in becoming a member click here.
Other helpful tips for self compassion with a vestibular condition
1.Treat yourself like you’d treat your best friend. Having symptoms is not your fault, don’t beat yourself up. Treat yourself how you would a friend going through the same struggle.
2. Finding kindness for yourself. This can be stating a phrase like “May I be kind to myself at this moment?” or “it’s okay, I’m here for you”. Consider imagining a pet or person and what you’d say to comfort them. Imagining them may also generate a feeling of kindness or warmth.
3. Remember that you are not alone. Part of the shared human experience is suffering. Say to yourself “I am not alone”. This shared experience connects us to so many others, people we know and strangers. All of this is part of being human.
If you’re interested in learning more, Melina recommends David Treleaven’s work “Trauma-Sensitive Mindfulness”. Learn more about his work here.
Disclaimer
Want to learn more about mindfulness, listen to recorded tracks to guide you through self compassion, other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Inflammation and dizziness
Have you tried traditional treatment for your vestibular condition or dizziness but feel like somethings missing? Dr. Emily Kostelnik discusses how unlocking the connection of inflammation and her body helped her find the missing piece of her vestibular treatment and management.
Meet Dr. Emily Kostelnik, PHD
Dr. Emily’s vestibular story
Dr. Emily Kostelnik is a clinical health psychologist and has her own personal experience with vestibular orders and dizziness. She has combined her personal and professional experience to assist others with vestibular conditions through Rooted Behavioral Education (link here) and her practice as a clinical health psychologist The Vestibular Psychologist (website here)
Follow her on instagram at rootedbehvaioraleducation and thevestibularpsychologist. She’s a wealth of knowledge and shares this on her social media accounts!
Dr. Emily also has a course on fucntional medicine, inflammation and alternative answers to dizziness. You can purchase the course here. Vestibular Group Fit members get a $75 discount so look in your premium content, or sign up for the discount ( you still save $15). If you’re unsure if this discount code is still active, email us and ask prior to purchase!
Dr. Emily Kostelnik was diagnosed with Superior Canal Dehiscence (SCDS) in 2018 with two surgeries to correct. In post partum, Dr. Kostelnik faced debilitating PPPD and VM.
Starting with more conventional treatment (VRT, Heal your headache diet, working with an otolgist), she noticed progress but still noted lingering symptoms. Medications were prescribed to address ongoing floating sensations, trouble with screen time etc but she felt like there was still something missing.
With the assistance of functional and integrative medicine doctors, Dr. Kostelnik researched more the possible role of inflammation and dizziness. This turned out to be an important part of her recovery and management strategy and she’s here to share what she’s learned. Overall she is dizzy free most days!
Yes, Dr. Kostelnik is dizzy from time to time, but again, is mostly dizzy free!
What is inflammation?
To understand inflammation in our bodies, we need to talk about our immune system. Our immune system defends our body from outside threats. Think bacteria, viruses, pollen, infections etc. Anything our body finds suspicious or potentially harmful, our immune system attacks.
Inflammation is the immune system’s response to a threat. Not all inflammation is bad, it is the first part of the healing process. Initially inflammation is good! It helps identify and surround the perceived threat to avoid damage to other tissues or further spread. This is done by the immune system leaking fluid and protective chemicals to the specific area. Typically, the next step is to clean out this area of the threat, and the acute inflammation phase is over and our body starts the next phase of returning to baseline.
When our body doesn’t start the next step and stays in the inflammatory phase, this can lead to chronic inflammation. In chronic inflammation, our body continues to respond like there is a present threat. A persistent state of chronic inflammation can feel like a decline in our health, like you’re never feeling like your best self.
Chronic inflammation can be a result of: chronic injuries, chronic infections, surgical implants, things we eat, the way we act (or don’t act…mindset is important!), sedentary lifestyle, our environment. A certain combination of factors, everyone is different, can begin to overwhelm our bodies and we then reach a state of chronic inflammation.
How does inflammation and dizziness fit together?
Research has found that people with vestibular disorders (acoustic neuroma, vestibular neuritis, vestibular migraine, BPPV, PPPD) and those with anxiety depression were associated with higher inflammatory markers. Inflammation can affect us all differently. For some, it causes dizziness, for other it may be migraine or a thyroid condition.
If our body is inflammed, and constantly trying to remove a threat, it impacts our body’s ability to function. This is additional energy, resources and stress on our body dedicated to increased inflammation. When our bodies are in this state, it’s hard to reach baseline or feel like your typical self.
3 Ways to that can help improve inflammation
- Exercise can help reduce inflammation in our bodies
- nutrition. our gut biome is super important. Eating inflammatory foods or having guy dysbiosis can impact inflammation in our body
- mindset. working on positive thoughts, or being with others to get a positive mood boost can work wonders for our body!
Mast Cell Activation Syndrome, Histamine, inflammation and dizziness.
We won’t go into much detail here, but you can find more on this via Dr Emily’s social media and in the interview with Dr. Emily and Dr. Madison for vestibular group fit members.
Mast cells release chemicals when a threat is perceived. Mast cells release many different chemicals, one of them is histamine. Too much histamine in our body can result in histamine intolerance and can contribute to chronic inflammation.
There’s a wide variety of opinion on this subject, and diagnostic criteria can be hard to accurately measure and meet. Even if you don’t meet the diagnostic criteria, you may still benefit from different management options. Talk if over with your doctor.
What about medications, supplements, antihistamines for inflammation and dizziness or MCAS?
Medications
- We can’t tell you what to take, that’s a conversation for your doctor. We’re big fans of taking meds when you need it and if that’s something you want to take. Medications aren’t a sign of failure and don’t have to be a forever thing if you don’t want it to be. Again, this is a hugely important conversation to have with your doctor! If they don’t support your preferences on this topic, find one that does if you can!
- It will be trial and error to find a med that works best for you. Meds are just one part of the treatment pie so keep in mind those other treatment options.
- if you’re on a med and happy with your current plan, great! Keep doing what you’re doing
Supplements
- everyone is different, some may benefit from supplements, others may not.
- this is very person specific, what does your body need and what are the routes to get it?
Anti-histamines
- again, what works best for you?
- some find elimination diets can be helpful, but this is a SHORT TERM SOLUTION. This can help determine why cells get overactive, or discover if there’s a personal connection in histamines, inflammation and dizziness for you
- anti-histamines may help symptom management, but long term use can have other health consequences including increased risk of dementia, or increased production of histamines to counteract the long term blockage. Again, do what works for you, have these conversations with your doctor. This may be a short term solution to dig deeper and find a longer term management plan!
How to Find and Functional Medicine Doctor
Find a list of all functional doctors here at IFM.org.
Reminder, functional doctors may have differing opinions on what they think is going on, and course of treatment. It may take a few to find the right fit or find the help that works best for you! Some may be helpful for inflammation and dizziness, you may find them helpful for other health conditions you don’t feel have been fully addressed!
Disclaimer
Want to learn more about inflammation and dizziness, and other vestibular tools from the experts and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
How to get through your ‘To Do’ List & Daily tasks with dizziness
Energy conservation (or pacing) is a way to listen to your body and strategize your day to get chores done while minimizing fatigue and dizziness as much as possible. Read on to learn how to get through your ‘to do’ list and daily tasks with dizziness, learn why it’s hard, ways to get it done today!
Phone battery analogy
Use a 0-100% battery meter to gauge your energy levels and dizziness on any given day. Keep in mind tasks you do will drain your batter, just like using your phone will drain it. Don’t let your energy battery (or phone battery) reach zero. It’s easier to charge when you’re at 70-80% than when you’re at 10%.
6 Tips & Tricks to pace with dizzness
Take a look at these 6 tips to strategize your day. Consider your energy/dizzy battery for the day and these tips to map out your day. Reminder, it’s okay to ask for help, to prep part of a task for a later day (like soaking dishes), or delegate to another family member or service.
Some days we have big plans to get things done, but we wake up with increase symptoms, fatigue, and a lower body battery. That’s okay, it’s not your fault and you are not a failure. Focus on what can be done, including self care to have the capacity for your list another time.

Household and daily tasks with dizziness: the breakdown
In this section we’ll cover some common household chores or daily tasks and discuss why they’re challenging and ways to make them easier.
Our premium content members also have guidance on movements and strength exercises to increase their tolerance to these tasks. Doing exercises and movement will make tasks easier to do in the future. Learn more here.
Dishes
Why it’s difficult:
- Repetitive body movement (from sink to rinse to drying rack)
- eye tracking
- standing balance
How to pace with dizziness:
- Use the dishwasher if available
- stack dishes to move more at once and reduce large/repetitive movements
- soak dishes to make cleaning easier and faster
- wash multiple items before rinsing to reduce movements
- try a suction glass cleaner to take some of the effort of off you.
Laundry
Why it’s difficult:
- lots of up/down movements
- busy visuals
- noise/smells/light depending on the environment
- mental energy to sort and fold
How to pace with dizziness:
- ask for help. Have family take their own pile of laundry to put away or fold
- do folding and sorting seated
- Make laundry your one task for the day. Break down the tasks to give yourself rest time
- don’t fold everything! I’ve started to keep clothes I don’t mind being wrinkly in fabric bins. When I sort laundry I can put my socks in the sock bin, delicates in the delicate bin, and workout shirts/shorts in their bin. Cuts down my laundry time and I realized how much folding I did for things that I didn’t care about needing to be folded.
Stairs
Why it’s difficult:
- physically demanding
- looking down
- visually challenging: seeing both near and far
How to pace with dizziness:
- Use the railing when available
- reduce trips by doing all tasks on the top floor and then going downstairs for tasks
- keep a basket at each end to place objects in that need to go up/down to avoid multiple trips. A great way to get others to help as well!
Cooking
Why it’s difficult:
- looking down
- balancing
- lots of turning and reaching
- tracking
- focus
How to pace with dizziness:
- use some prepped foods like pre cut veggies
- do food prep in sitting when able
- Find simple recipes, The Dizzy Cook is an awesome resource, her cookbook is here
- have some easy frozen and pre baked meals
- use a slow cooker
Computer time
Why it’s difficult:
- tracking and scanning
- head position and posture
- mental fatigue and concentration
- light sensitivity
How to pace with dizziness:
- ergonomics for better computer posture (some extra tips for set up here)
- avalux glasses (code: VERTIGODOC will you get $25 off) or other blue light blocking lenses
- taking breaks with the 20-20-20 rule
Reading
Why it’s difficult:
- mental fatigue and concentration
- tracking and scanning
- head position and posture
How to pace with dizziness:
- audiobooks when able
- use your finger to help track the line you’re reading
- take breaks
Showering, Grocery Shopping, Escalators, Elevators, the dentist/hair dresser, cleaning the house, gardening and more!
Learn why wall these tasks are challenging, ways to get these tasks done now and products that help, and how to work on movements to improve all of the tasks listed today! All of this and more is included in our supportive community at Vestibular Group Fit! Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
Conquer vestibular migraine: a beginners guide
Here is a beginners guide to vestibular migraine. We’ll cover the difference between migraine, vestibular migraine, management tips and tricks, and when to start vestibular rehabilitation (VRT).
What is migraine? How is vestibular migraine different?
In general, migraine is a neurological disorder and has various symptoms that can be present. Here is a list of some common symptoms associated with migraine:
- head pain (typically experienced on one side, near the eye/temple region, but not always)
- vertigo, imbalance, and dizziness
- light sensitivy
- sound sensitivity
- smell sensitivity
- nausea/vomitting
- neck pain
- ear ringing/tinnitus
- visual changes
- tingling
- and more
Migraines act differently with each person. A common misconception is that a migraine is only a bad headache, or if you know someone with migraines and their symptoms are different than what you experience you think “oh well I don’t have migraines because they’re nothing like my friends”. If it’s impacting your life, it’s worth talking to a medical provider about!
Vestibular migraine
Vestibular migraine accounts for 3% of all migraines. This subtype of migraine has specific symptoms relating to the vestibular system (vertigo, imbalance, dizziness, brain fog, feeling “off”, lightheadedness etc).
The International Classification of Headache Disorders criteria for vestibular migraine are:
- At least 5 episodes of vestibular symptoms of moderate or severe intensity lasting 5 minutes to 72 hours
- Current or previous history of migraines with or without aura according to the ICHD classification
- One or more of the following migraine features with at least 50% of vestibular episodes:
-
- Headache with at least 2 of the following characteristics
- One-sided location, pulsating quality, moderate or severe pain intensity; photophobia or phonophobia
- Visual aura
- Not better accounted for by another vestibular or ICHD diagnosis
click here for the research article that outlines this criteria.
The big thing to remember here is that not all vestibular migraines have head pain/headaches. Headache can be present, as well as the other symptoms on the list above in addition to vestibular symptoms.
Phases of migraine
- There are 5 phases to migraine. Again, everyone can experience these phases differently, but are important to know to better identify how your body responds to a migraine event so you can act quickly when you begin to see signs of a migraine for best results.
The 5 phases are:
- Prodrome
- Symptoms that occur in the beginning of an attack. Can last hours to days
- Aura
- neurological symptoms that occur right before an attack. Can last 5min-60min
- Attack
- The most severe symptoms, lasting hours to days.
- Postdrome
- The end of an attack, gives you a “hangover” feeling. Can last hours to days
- Interictal
- Symptoms that are experienced between attacks (quick spins, fatigue, light and sound sensitivity are a few). This is due to the underlying migraine condition and where vestibular rehabilitation therapy (VRT) can be helpful. But it’s also very important to get the migraine under control before heading into VRT, more on this later!
When to start Vestibular Rehabiliation (VRT)
VRT is beneficial in addressing residual symptoms after migraine attacks, or the interictal symptoms experienced in day to day life. VRT is most effective when attacks are mostly under control. If you’re having multiple attacks in a month, or you’re having a hard time getting symptoms under control, VRT may not be appropriate at that time. A couple of sessions may be helpful for education to try various methods to get symptoms under control, or addressing neck pain through gentle stretching, manual work, postural and ergonomic education).
VRT is most beneficial when your migraine is under control. Using habituation principles to improve interictal symptoms is best done when your vestibular migraine is under control. If your migraine and symptoms aren’t well managed, trying to do VRT is like throwing gasoline on an already raging fire and hoping it burns out. This is why VRT can make you feel worse. It’s important to have a therapist familiar with vestibular disorders and vestibular migraine to guide and dose your VRT appropriately.
What should I do when I have a vestibular migraine attack
If you begin to feel an attack coming on, you want to initiate your plan as soon as possible to try to stop th eattack or minimze the severity or time of symptoms. This may look like:
- Acute meds prescribed by your neurologist
- magnesium
- ginger
- grounding and breath work
- gentle walking
- water
- electrolytes
- Cefaly or GammaCore
- essential oils
- icepack/headache hat
Vestibular migraine management
- Start with the basics:
- eating meals regularly
- consistent sleep
- hydration
- Gentle, daily movement
- Mindfulness and mindset work. Stress can be a big migraine trigger!
- Consider blue light glasses, ice packs/headache pack, educational books (found more in depth here)
- Research backed vitamins and supplements for migraine (full list here). Vestibular Group Fit members get 30% off their fullscript orders!
- Talk to a neuroglist to see if you fit a vestibular migraine diagnosis. Discuss a plan for you regarding preventative, acute and rescue medications.
- Track large symptom days to find patterns. (migraine buddy is a helpful app for this)
- Diet and hormones can also be involved. More on diet here and here and here; more on hormones here and here.
There’s a lot of great content on tis website for vesitbular migraine, I tried to include most of it here but might have missed some. Vestibular Group Fit is a great place to find all this information presented to you in one spot with excellent resources, with a community of others to provide their own experience, advice and guidance for symptom management, lifestyle changes, and support with movement.
Disclaimer
Want to learn more about vestibular migraine management and be a part of a supportive community to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
3 ways Somatic Therapy can help dizziness
Learn how somatic therapy can help dizziness with psychotherapist Kate Schwab, LCSW. We’ll cover what somatic therapy is, the benefits, and tools to get started today.
Kate Schwab, LCSW is a licensed clinical social worker and psychotherapist. In vestibular group fit, Dr. Madison and Kate talk about how somatic therapy can help dizziness and tools that are helpful in supporting your body.
What is Somatic Therapy
Somatic therapy combines psychology, neuroscience, ethology, physiology, indigenous healing practices, and medical biophysics. Guidance of somatic therapists assist you in learning what your body needs to feel supported.
3 parts of somatic therapy involve:
- Nervous system activation and overwhelm
- Pacing
- Support tools
We’ll take a look at each of these parts to learn how somatic therapy can help dizziness. More information and a recorded interview with Madison and Kate can accessed with a premium account.
How is Somatic Therapy different than Acceptance and Commitment Therapy (ACT) or Cognitive Behavioral Therapy (CBT)?
ACT/CBT are talk therapies type and focus on behavior. Both are symptom management focus. ACT brings in more mindfulness work: what are your behaviors and beliefs and changing those. With somatic therapy, it’s less symptom oriented and more of ‘what’s happening for you internally?’. We are looking at WHY those symptoms are there and deeper work. These areas cover different parts, so if you’ve had ACT or CBT therapy, you could benefit from somatic therapy. Keep reading to learn how somatic therapy can help with dizziness in its unique way.
Who could benefit from Somatic Therapy?
Most people can benefit from this work, and there are many reasons we experience trauma responses. Chronic illness can be traumatic and so in general somatic work can be really useful!
Nervous System Activation and Overwhelm
When first experiencing pain or dizziness, we begin to try everything and anything to make it go away. This urgency can lead to desperation, feeling overwhelmed and hyper vigilant of what we’re experiencing. This heightened state ramps up our sympathetic nervous system- the “fight flight or freeze”. This is not a state we are meant to be in for long periods of time,and normally kicks in when there is an external threat. When the threat is external, like a sudden loud noise or dark looming figure, this is extremely helpful to get us out of that area and to safety. In the case of dizziness, the perceived threat is internal, so how do we get to safety? This is where somatic therapy can help.
This is so so common in dizziness, check out this article on the dizzy anxious cycle and Dr. Emily Kostelnik with Rooted Behavior Education for more on this as well.
Back to how somatic therapy can help with dizziness. Learning how our own body and nervous system begins to ramp up and “activate” helps us identify what our body needs to get through these situations and move towards health and homeostasis. Everyone is different, and each situation is different.

If we ignore these signs, or don’t have the tools to help support what our body is telling us, we can reach a point of overwhelm and our body shuts down on us. Pacing is the practice of identifying these activations, and working on tools to assist your body, a major part of what Kate and other somatic therapists are amazing at!
Pacing
Pacing involves going SLOW. This is not easy and takes practice. This makes us think about the exact moment we are in and what our body is experiencing. Go into a quiet room and focus on moving towards health. Focusing on what you’re feeling right now, what your body needs right now. This is abstract and hard, which is why lovely people like Kate are here to help guide you further. Pacing helps identify what you’re experiencing, and getting support systems in place. This is how somatic therapy can help with dizziness.
Over time and with practice, the goal is you start to learn more about your body and have tools to support it. Pacing helps you be more aware of your window of tolerance. It’s okay to have nervous system activation, people like Kate help you to identify and work through it. If you aren’t in touch with your body, it’s hard to move along various activation states tolerably.

Support Tools, Avoiding Hyperawareness, Derealization/Dissociation
It’s important to check in with your body with chronic conditions and symptoms to avoid doing too much, making it easy to become hyper vigilant of what you’re feeling.
Try and know that you know how to handle this, and you’ve filled your prescriptions, and you can call your doc if needed, you have a support system, and at the same time you need to let your brain set it down and enjoy the moment that you’re in. This is hard and takes repetition and practice.
What about derealization or dissociation?
These come with the feeling like you aren’t real. Like you’re watching your world through a TV. Feeling disconnected or viewing the world from a glass plane. These can be survival mechanisms (and that’s not a bad thing!) but ways to try to shake this are:
- Breathing (box breathing or 4 counts inhale, 8 counts exhale. Hold briefly before repeating)
- talking out loud to yourself “I’m okay I am present, I am here”
- can you put on a podcast to laugh at, music to sing or dance to?
Give these a try, did it help? These are a few of the ways somatic therapy can help dizziness, derealization and dissociation.
Contact info
Follow Kate for ongoing education or reach out if you have questions or are interested in working with Kate to see how somatic therapy can help dizziness, chronic pain and more! Click here to reach Kate’s website.

Want to learn more about tools, how somatic therapy can help dizziness, and other vestibular tools to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.
5 Main Audiology Tests for Vestibular Disorders
With vestibular audiologist Dr. Alexandra Smith, Au.D, CCC-A, F-AAA.
Dr. Alexandra Smith is based in Santa Fe, NM (you can find her clinic here) and works to identify, diagnose, treat and prevent various diseases, injuries or defects of the ear. Audiologists are also able to assist their clients with maintaining good hearing and can assist with hearing devices. Dr. Smith perform audiology testing for vestibular disorders and is going over them in more detail to help you better understand your test results and know what to expect. If you think you’d benefit from audiology testing for vestibular disorders, talk to your doctor about comprehensive audiology testing.
This blog post covers some content Dr. Smith covers with Dr. Madison Oak, vestibular physical therapist for our vestibular group fit members. These tests are common when evaluating for vestibular disorders but aren’t always well known or explained. Read below to learn more about audiology tests for vestibular disorders and what they can help tell you about your vestibular condition.
What is a vestibular audiologist?
A specialty within audiology which includes:
- Hearing and tinnitus evaluations
- Surgical implant care
- Vestibular evaluation
- Select vestibular treatments (like the epley maneuver for BPPV)
- Diagnostic tests which we’ll go into more detail below! (ECOG, audiogram, VNG, brain wave testing, positional testing and more)
Using audiology tests for vestibular disorders can be another piece of information to consider with other testing (MRI, physical therapy, occupational therapy, ENT, Neurology etc) to best determine a plan of care to manage your vestibular condition.
What is the role of a vestibular audiologist?
What does audiology testing and vestibular disorders have to do with each other? Anatomically, our inner ear has both a spatial awareness system (the vestibular system) AND hearing portions (the cochlea) that make up the inner ear. The nerve that connects our inner ear to the brain also branches from the same nerve to reach both of these sections. It is also common to have other ear symptoms or hearing changes with vestibular conditions, so it’s important to get testing done by a specialist in the hearing portion of our inner ear, an audiologist!

What are the 5 main audiology tests for vestibular disorders?
Common audiology tests for vestibular disorders include:
- VNG (Videonystagmography exam)
- Caloric testing
- ECOG (Electrocochleography exam)
- VEMP (Vestibular evoked myogenic potential)
- Audiogram
Below, we’ll go into more detail on what these tests measure, what to expect, and how these tests can help with vestibular diagnostics.
VNG (Videonystagmography exam)
- Goggles are worn to measure and track eye movements using special software and is tracked on a chart
- Wearing the goggles, the audiologist will perform an oculomotor exam (tracking targets, saccades/looking between multiple targets other eye movements)
- Positional testing such as the Dix hall pike (for BPPV testing)
- caloric testing, read on to learn more about this one
- VNG can help determine any positional dizziness like BPPV and identify any central signs that may warrant a referral to a neurologist, or peripheral signs that could point to a vestibular condition
Caloric testing
- Done with air or water, each ear gets 1 minute of warm and 1 minute of cool air/water
- The temperature of the warm and cold air/water is mild. This temperature change stimulates your vestibular system. This can cause uncomfortable sensations of movement or rotation.
- It is normal to feel dizzy for part of the test and it will go away. All you have to do is keep your eyes open!
- The stimulation of the vestibular system causes the dizzy sensation and eye movements (nystagmus- more on that here)
- These eye movements are being measured with infrared video goggles. The left and right ear are compared to see if the movements are symmetrical.
- If the left and right ear are asymmetrical, this could indicate a unilateral vestibular weakness or vestibular hypofunction (you can learn more about this here)
You are in control and can stop at anytime, it is NOT AN ATTACK.
ECOG (Electrocochleography exam)
- A brain wave test that looks for increased fluid pressure in your endolymphatic sac in your inner ear (indicative of meniere’s disease)
- NOT a test in isolation of meniere’s disease-more accurate in the middle of an episode but more people don’t get into a clinic for testing during an episode
VEMP (Vestibular evoked myogenic potential)
- Cervical and ocular VEMPS are cVEMP or oVEMP
- Testing otolith function ( the utricle and saccule)
- Analyze the two branches of your vestibular nerve.
- Can see if one nerve is stronger than the other or if one side is weaker
- Can test for 3rd window syndrome like superior canals dehiscence syndrome
- Laying down on the table, one head movement and one eye movement.
Audiogram
- A hearing test, typically for first test you get in a audiologists office
- Can be very helpful in what’s going on and even help address what you’ve been experiencing
- Can tell you if you have hearing loss and where (what type of frequencies), and tympanic reflexes that can let us know about any ear pressure that man be going on
- Labyrinthitis will cause hearing loss
- Meniere’s disease also causes low frequency hearing loss on the affected side
- Age related hearing loss tends to be in both ears and at higher frequencies.
Can you have normal testing and still have a vestibular disorder?
YES! Certain vestibular conditions will not show up on this testing. Migraine will not show up on MRI, CT scans, ECOG VEMP or VNG or audiograms. These tests can still be helpful for these conditions that require a diagnosis of exclusion to rule out other conditions that these tests can reveal. Audiology tests for vestibular disorders can help lead us to identify specific diagnoses. If testing comes out normal, audiology tests for vestibular disorders can also help consider other diagnoses that would show normal testing.
Audiology tests for vestibular disorders is one piece of testing to be considered with other providers testing and listening to what you’ve experienced. Listening to your experience and looking at all the test results can help get the right team of providers (OT, PT, Neuro, ENT) in your corner to start your healing journey. It’s natural for this team to change slightly, or change focus for periods of time with certain providers based on your needs. Keep your team in the loop so they can help adjust accordingly, they’re here to help YOU.
Want to learn more about vestibular testing, ear pressure, tinnitus and other vestibular tools to get back to your daily life? Find out more at this link: https://tvd.flywheelstaging.com/about-group/
Disclaimer:
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.