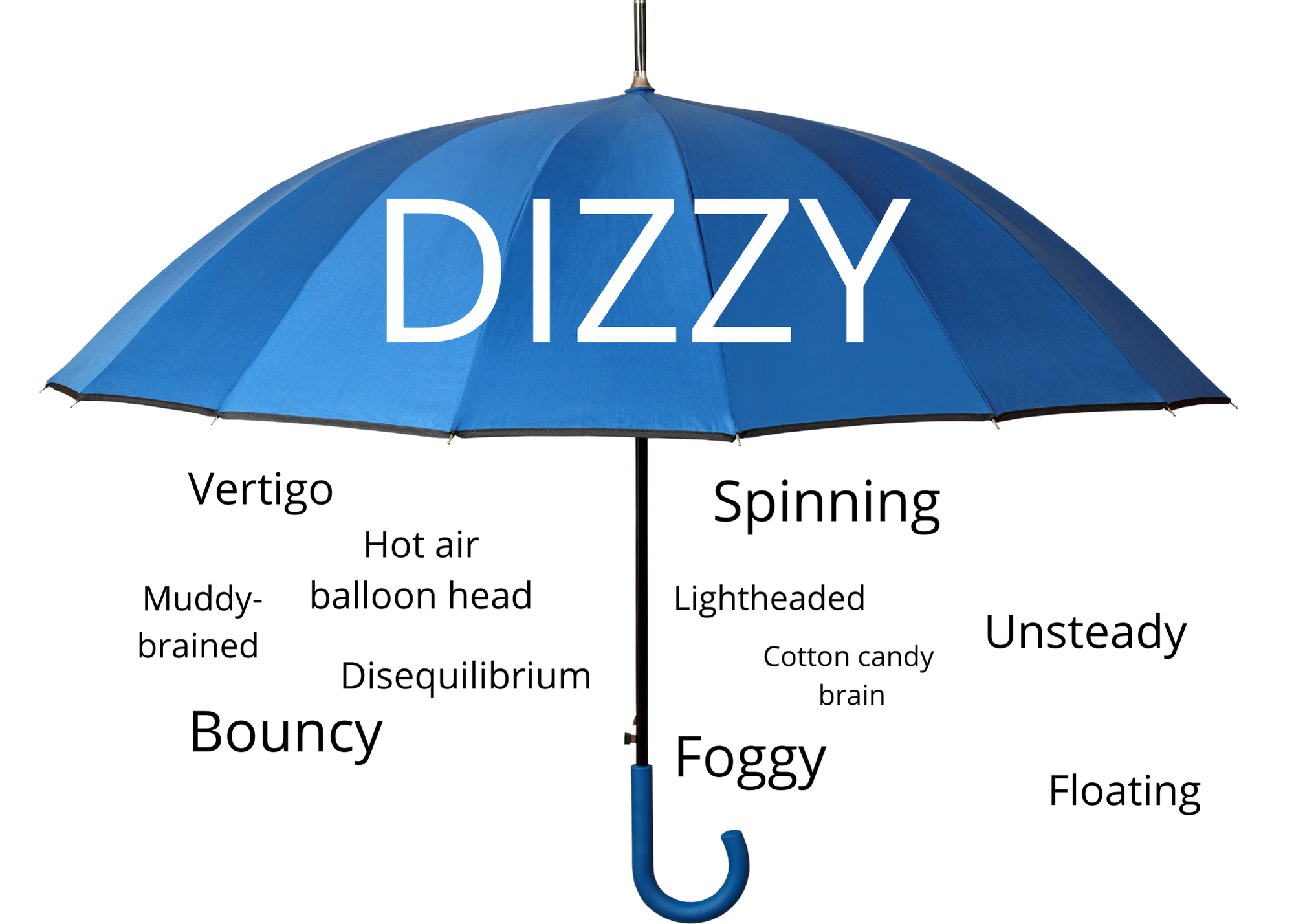
Join Vestibular Group Fit
Learn how to thrive with your Vestibular Disorder.
Disclaimer: This advice is not meant to be a substitute for advice from a medical professional regarding diagnosis, prognosis, or treatment. Always seek advice from your physician, physical therapist, or other qualified healthcare provider with questions you may have regarding a healthcare condition. The information of this website, including but not limited to text, graphics, videos, images, and other materials are for informational purposes only. Reliance on the information on this website is solely at your own risk.
Amazon Affiliate Disclaimer: As an Amazon Associate, I earn from qualifying purchases.
Menu
Articles
Contact Us
- [email protected]
- Monday - Friday 08:00 - 19:00